
Ed Reed/Mayoral Photo Office
Mayor de Blasio displays a map of testing results in the city as of March 27. Access to testing is just one of the possible healthcare disparities that might have contributed to the apparent racial skew in the city’s death rate.This story originally appeared in English. Esta historia se publicó originalmente en inglés. Read the Spanish version here. Lea la versión en español aquí.
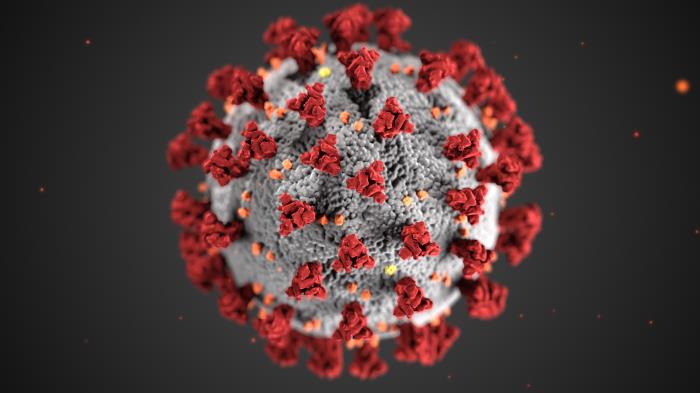
As the rate of new coronavirus cases continues to slow, the picture of its racial and ethnic impact is shifting. The first snapshot released by the city in early April showed a significant overrepresentation of Latinos among the dead, and a more modest skew toward Black deaths. The latest numbers reverse that: the death rate is now higher among Black New Yorkers.
The thread that runs through all the numbers so far, however, is that Blacks and Latinos comprise a larger share of the dead than they do of the New York City population. The latest figures have Blacks dying at a rate of 127 people per 100,000, Latinos perishing at a rate of 114 per 100,000. The rates for Whites and Asians were 64 and 52, respectively.
The explanation for the disparity seems obvious: Blacks and Latinos have higher rates of poverty, and therefore are more likely to have suffered from underlying health conditions that made them more vulnerable to COVID-19.
There’s been less discussion of how those underlying conditions and longstanding inequalities actually translated into deaths, or about other factors that might help to explain the racial disparities characterizing COVID-19’s impact.
Not just poverty, but history
The mayor and health commissioner pointed their fingers at poverty and inequalities factors during the press conference on April 8th at which they disclosed that COVID-19 was disproportionately killing African Americans and Latinos.
Latinos, whose 2016 poverty rate in New York City was 23.9 percent, and Blacks, whose poverty rate was 19.2 percent, are more likely to live below the poverty line than Whites, who had a 13.4 percent poverty rate that year. But Asians actually had the highest poverty rate in the city that year—24.1 percent—and that group has had the lowest death rate from COVID-19.
According to social scientists, understanding why Blacks and Latinos are being disproportionately affected by COVID-19 requires acknowledging historical inequities.
“Neighborhoods with a high proportion of African Americans due to structural policies and practices, such as redlining, eviction practices, and disinvestment in low income neighborhoods, which has led to residential segregation in such areas, may be most vulnerable to the COVID19 pandemic,” says Dr. Camille Clare, associate dean of diversity and inclusion at New York Medical College.
As of April 23rd, the Bronx has the highest rate of positive cases: 2,168 per 100,000 residents in a borough in which 56.4 percent of people identified as Hispanic or Latino, 43.6 percent of people identified as African American, and where 27.3 percent of people lived in poverty, based on Census data.
In regard to social and economic conditions a 2017 Health of Latinos in NYC report says that “structural racism in Latino communities creates concentrations of poverty, unemployment and poor education, which limit access to resources that promote health and prevent illness. These factors can also increase stress and lead to poor health outcomes.”
Underlying health concerns
On April 22, the Journal of the American Medical Association published a study confirming what physicians nationwide have noted anecdotally: the most common comorbidities for hospitalized patients with coronavirus are diabetes, obesity, and hypertension.
Dr. Martha A. Dawson, national president of the National Black Nurses Association, explains the way underlying conditions play out within African American and Latino communities this way: “What would best resist a tornado: a strong brick house or a trailer? Having higher incidents of underlying conditions places African Americans and other underrepresented groups at a disadvantage in the US health system.”
Latinos overall, compared with other New Yorkers, have a higher prevalence of chronic conditions such as diabetes, 17 percent vs. 10 percent; and obesity, 29 percent vs. 20 percent. A similar trend can be found among NYC public high school students who are more likely to be obese: For Latinos, it is 15 percent, compared with non-Latinos, 11 percent.
Blacks adults, meanwhile, had a premature death rate due to heart disease that was 1.8 times that of White adults, and 2.1 times that of Latino adults from 2011 to 2015, according to the NYC health report. “Heart disease is twice as likely in very high-poverty neighborhoods as in lower-poverty neighborhoods; Black women are 2.4 times as likely to die from heart disease as White women and 5.6 times,” reads NYC health report.
As Mary Travis Bassett, former New York City health commissioner and current director of the FXB Center for Health and Human Rights at Harvard University, says, many of the health problems Latinos and African Americans are dealing with are not genetic in nature.
For example, “diabetes is a chronic disease related to income; it has social roots. Processed food tends to be cheaper than healthier options,” says Bassett.
Environmental factors influence underlying health in a number of ways. “The rates of what we call cardiometabolic syndrome (e.g., diabetes, hypertension, stroke, etc) are higher among Black and Latinx communities, as compared to other communities,” says the Council on Black Health. “Increased rates of cortisol, a stress hormone and the body’s natural alarm system that manages the ‘flight or fight’ instinct all humans have, are the main cause for cardiometabolic syndrome.”
Nationwide, as Dr. Clare highlights, “Black Americans were already three times more likely to die from asthma-related causes in 2014, according to the US Department of Health and Human Services. Living in neighborhoods with more air pollution is likely a contributing factor: Blacks were 75 percent more likely to live in places bordering a polluting facility like a factory or refinery compared to other Americans, according to a 2017 report by the NAACP and Clean Air Task Force. They’re also exposed to air that’s 38 percent more polluted in comparison to white Americans, the report found.”
Research is ongoing into specific ways that racial skews in environmental risks and underlying health conditions—as well as the treatments for those ailments—might increase COVID risks.
A pre-print study by the Harvard University T.H. Chan School of Public Health concluded that “a small increase in long-term exposure to PM2.5 [micro dangerous particles in air] leads to a large increase in COVID-19 death rate, with the magnitude of increase 20 times.”
This novel virus “uses the same biological mechanism as the proteins used in high blood pressure medications (angiotensin converting enzyme-2 or ACE2 receptors),” explains the Council on Black Health though the Council adds that “while it is unknown if this relationship is the cause for this increase among Black and Brown communities, this relationship must be explored more.”
Healthcare access
As City Limits reported early this year, Latinos have the highest rates of uninsured population (followed by Blacks) in both the country and in the New York metropolitan area. The rate remains high despite Latinos having the biggest decline in uninsured population numbers from 2009 to 2015, thanks to the Affordable Care Act.
Among Latino communities living in the city, rates of uninsured populations among the five largest Latino nationalities vary, according to the report by the Center for Latin American, Caribbean, and Latino Studies at the CUNY Graduate Center. More than a third of Mexican New Yorkers were uninsured in 2015, compared with a quarter of Ecuadorians, 15 percent of Colombians, 11 percent of Dominicans and just 6 percent of Puerto Ricans.
As these numbers show, there is a significant variation in access to health insurance coverage between US-born Latinos and foreign-born Latinos. The 2017 health report found that a higher percentage of Latinos born outside of the US are uninsured (30 percent) compared with US-born Latinos (8 percent).
Even though healthcare is not considered a government benefit under the new public charge rule, Latinos who are immigrants and who are planning to become citizens or residents may not seek health care out of fear of becoming ineligible. Earlier this month, the city’s current health commissioner, Dr. Oxiris Barbot, expressed concerns about the role that might have been played by xenophobic rhetoric and policies. “The overlay of the anti-immigrant rhetoric across this country, I think has real implications for the health of our communities.”
Blacks, meanwhile, face documented barriers to getting adequate care.
“Segregated care based on insurance coverage has been well documented, such as there are ‘Black/low socioeconomic serving’ and ‘White/high socioeconomic serving’ hospitals which may be resourced differently. As it pertains to COVID-19, differences in the rates of testing or the ability for universal testing play a part,” says Dr. Clare. Thus she proposes that “when screening questions are used to determine who will undergo diagnostic testing, high-risk groups including persons who are African American, Latinx, American Indian/Alaskan Native should be assigned a high priority risk score to enable testing.”
Employment and risks
There is also a racial overlay affecting who works in careers where they are likely to contract COVD-19.
The Citizens’ Committee for Children of New York (CCC), looked into communities with the most coronavirus-related deaths, compared that to the data they have on labor and found relatively high rates of employment in industries where exposure to the public is common—for instance, that about “one in five residents in West Queens work in hospitality, accommodations, and restaurants; and about one in five residents in Southeast Queens work in health care.”
Jennifer March, the CCC’s executive Director, says that “communities with residents experiencing higher rates of COVID-19 are marked by high rates of poverty, overcrowded housing, lower rates of health insurance coverage among adults, lack of access to preventive care, and have a large share of the workforce working in essential services.”
Ana Abraido-Lanza, Vice Dean of the School of Global Public Health at NYU, says that compared with non-Latino Whites, “higher percentages of Latinos work in service sector occupations that are classified as ‘essential.’ They are not able to work from home, which exposes them to the coronavirus.”
The story is similar for Blacks. Nationally, only 16.2 percent of Hispanic workers and 19.7 percent of Blacks can telework, according to the Economic Policy Institute.
Closely related to one’s type of work—and ability to telecommute—is whether sick-time is a viable tool. In April, a study by the Pew Research Center found that around half of Latinos say they have taken a pay cut, lost a job, or both, due to COVID-19, compared with 33 percent of all U.S. adults. So, “Latinos who are experiencing symptoms might delay seeking care due to fear of missing work,” says Abraido-Lanza.
The city has now moved to run more testing in African American and Latino communities. On April 17th, the city opened five community testing sites around the city, “all run through our public health system, Health + Hospitals, and directly serving those hard hit areas,” de Blasio said.
Unanswered questions
While possible explanations for the disparity in death rates abound, clear answers are not yet at hand. “To date, there has been little progress in identifying the main factors,” says Abraido-Lanza. “Research is needed to better understand the disturbing trend of higher death rates among NYC Latinos compared to non-Latino whites,” she adds.
According to Josiemer Mattei, the Donald and Sue Pritzker Associate Professor of Nutrition at Harvard T.H. Chan School of Public Health (who was not involved with the pre-print study), “the general answer is that we do not have a clear understanding of the situation around minority populations. So far we can speculate, mainly based on pre-existing inequities that may be driving the disparate numbers of COVID-19 among Latinos now.”
Some wonder if, for non-English-speaking Latinos, the language barrier has been a factor. If so, it would not be the first time. The 2017 health report says that “compared with non-Latinos, a higher percentage of Latinos report needing medical care but not getting it (12 percent vs. 9 percent).”
“The Health Department is working to ensure that provider and support teams look like and speak the languages of the communities they serve, including Spanish,” says Department of Health and Mental Hygiene.
Another unanswered question is whether people with health insurance get tested for COVID-19 more frequently than those who don’t have it in NYC, and how this might have been affecting Blacks and Latinos. For example, the New York Post found that coronavirus testing has been done on two-thirds of the 30 ZIP codes where either Whiter or wealthier people live.
“We have heard of anecdotal data where people have described trying to receive tests from multiple hospitals and being denied them. Early on in the pandemic, there were strict protocols of who could receive testing, thereby limiting access for Black people who may have not been around people who had received testing,” says the CBH.
Even the city’s latest snapshot of the coronavirus’s impact is based on partial information: Racial and ethnic information exist in only 40 percent of cases where people tested positive for COVID-19 but were not hospitalized, but is present in 92 percent of deaths.
The frustrations expressed by health advocates and journalists over the lack of information about racial impact earlier in the crisis could pave the way for better tracking in the future—to chart the course of pandemics and everyday disparities in health access and outcomes.
“This is an opportunity to highlight the need for regular collection and analysis of all relevant patient healthcare and outcomes data by race, ethnicity, language and [sexual orientation and gender identity],” says Dr. Clare.









12 thoughts on “More Questions Than Answers About the Racial & Ethnic Skew in COVID-19 Deaths”
The unintended consequences of corruption are right in front of us. THIS Mayor has closed hospitals and worked with developers to build .. build .. build. His donations from the real estate industry are outrageous. He has been in public office for over 20 years and now is preaching to us…He needs to look in the mirror when this is over and quickly get out of the way.
Which hospitals has he closed?
All of them essentially. Only allowing them to be available for treating a disease that you’re less likely to get hurt by than you are by simply driving your car to work and hasn’t even infected more people than the normal season flu? By the actions he’s taken, a large portion of doctors and nurses have been furloughed bc they were effectively shut-down by this dumb ass, race-bating piece of trash posing as the mayor of NYC.
Your comment has literally no basis in fact. Prioritizing hospitals to deal with a particular disease is not equivalent to closing hospitals, and emergency cases of other sorts are still being treated. And in seven weeks this illness has killed 10 times as many people as the flu does in an entire year.
Thank you x3 (so far), Jarrett Murphy.
Reply to B.M.:
Are you the same B.M. who worked with me at CHB back in the 1970’s and 1980’s?
Until we get a reliable racial breakdown of Covid-19 cases, the racial breakdown of deaths is an inaccurate measure.
Deaths by borough [4-24-2020] –
Boro || deaths || as % of boro cases || as % of NYC deaths
Bronx || 2342 || 7.127% || 21.804%
Brooklyn || 3190 || 8.237% || 29.699%
Manhattan || 1390 || 7.616% || 12.941%
Queens || 3304 || 7.292% || 30.761%
SI || 515 || 4.717% || 4.795%
NYC || 10741 || 7.353% || 100.000%
No it’s not. If people are dying of a disease at a disproportionate rate, it doesn’t really matter whether there is a similar skew in overall cases. What are the implications if those numbers are different? Under one scenario, Blacks and Latinos are getting the case less often than Whites but dying of it more–which could indicate some issues in treatment, but doesn’t change the story of disparity. In the other scenario, Blacks and Latinos get it more often and die from it more often, which is still a problem.
Really? Is there no low that these people won’t stoop to when it comes to playing the race card no matter how outrageous and ridiculous the reason behind doing so? This is the crap that’s slowly destroying the moral fiber of what was once the greatest nation in human history (that’s right, we longer get to say that when half the citizens think this idiotically).
Acknowledging statistical reality is not playing the race card. And when would you say the moral fiber of our nation was at its highest point?
Except when the statistical reality is such a huge twist of the truth you need to seek shelter in a basement.
Obamacare saved latinos but not black people because of racism?????
You are a huge part of the problem. Stop blaming skin color for everything in life.
The latest numbers:
Cases per 100,000
Asian 2279.88
White 3141.19
Black 3276.73
Latino 4363.31
Hospitalizations per 100,000
Asian 409.96
White 459.25
Black 875.25
Latino 938.32
Deaths per 100,000
Asian 120.68
White 139.39
Black 258.09
Latino 278.87
The data clearly indicates a racial skew.
I don’t recall mentioning Obamacare, or blaming skin color for everything in life. We are just reporting the reality of a racial skew in COVID-19 deaths.