A Commonwealth Fund survey of 18,000 older residents across 10 different countries found that American seniors were more likely to have depleted their savings, lost income and gone without vital medical care during the pandemic.

Adi Talwar
Masked residents play an early evening games of dominoes in one of the tree canopied seating areas at Serviam Gardens, an affordable housing complex for seniors in the Bronx.Older Americans have suffered greater hardships during the COVID-19 pandemic—including financial struggles and disrupted medical care—than their counterparts in other wealthy nations, a new report found, disparities that are particularly stark for Black and Latino seniors in the U.S.
The Commonwealth Fund surveyed more than 18,000 adults over 65 across the U.S. and 10 other countries, asking about their experiences during the pandemic when it came to economic security, their feelings about the COVID-19 vaccine and access to medical care and other support services. The survey was conducted between March and June of this year, and included participants in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the United Kingdom.
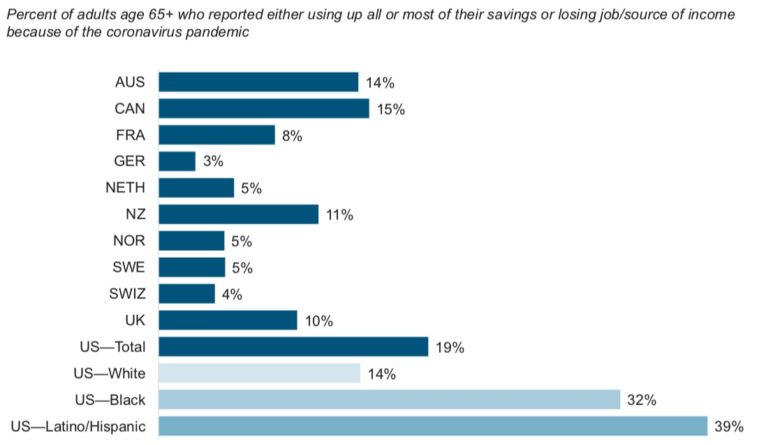
It found that nearly one in five of the U.S. participants had lost their job or depleted all or most of their savings because of the pandemic, more than any other nation surveyed. Black and Latino American seniors were the hardest hit, with 39 percent of Latino and 32 percent of Black participants reporting those economic hardships, compared to 14 percent of white seniors who did.
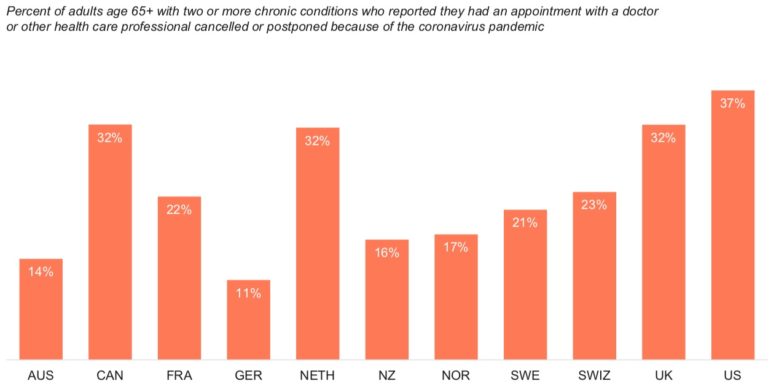
The U.S. participants also reported more disruptions to their regular medical care than those in other countries. The survey asked older adults with multiple chronic conditions—ailments like diabetes, high blood pressure, heart disease and depression—if they had appointments with health care providers cancelled or delayed because of the pandemic. In the U.S., 37 percent of respondents reported such disruptions in care, followed by those in Canada, The Netherlands and the UK, where that number was 32 percent.
Nearly a quarter of the American seniors surveyed also experienced problems accessing other support services during the pandemic, saying they were unable to get needed help with daily tasks like housework, shopping, medication management and preparing meals. This was exceeded by participants in the UK and Canada, where 30 and 31 percent of respondents, respectively, reported such access issues.
Older adults in the U.S. were also the most likely to say they don’t plan to get vaccinated for COVID-19, with the number one reason for skipping the shot being that they “do not trust the government to make sure the vaccine is safe.”
The survey’s authors say the findings reveal how the coronoavirus pandemic’s impact on older adults “goes beyond a higher risk for serious infection.”
“Our leaders can do more to address these disparities,” David Blumenthal, president of The Commonwealth Fund, said in a call with reporters on Tuesday. He attributed several of the disparities to the lack of universal health care in the U.S. compared to other nations. While American seniors have access to Medicare, there are often coverage gaps in the public insurance program, with many patients forced to pay out of pocket for supplemental insurance.
“We can make healthcare more affordable for seniors,” he said, recommended that American lawmakers focus on capping out-of-pocket costs for Medicare recipients and expanding the program to cover more health services, like dental, vision and hearing.
New York City is home to approximately 1.2 million residents older than 65, accounting for more than 14 percent of the city’s population, according to Census data estimates. A recent report from the Brookdale Center for Healthy Aging at Hunter College and nonprofit organization LiveOn NY estimates that by 2040, more than 1 in 5 New Yorkers will be aged 60 and up.