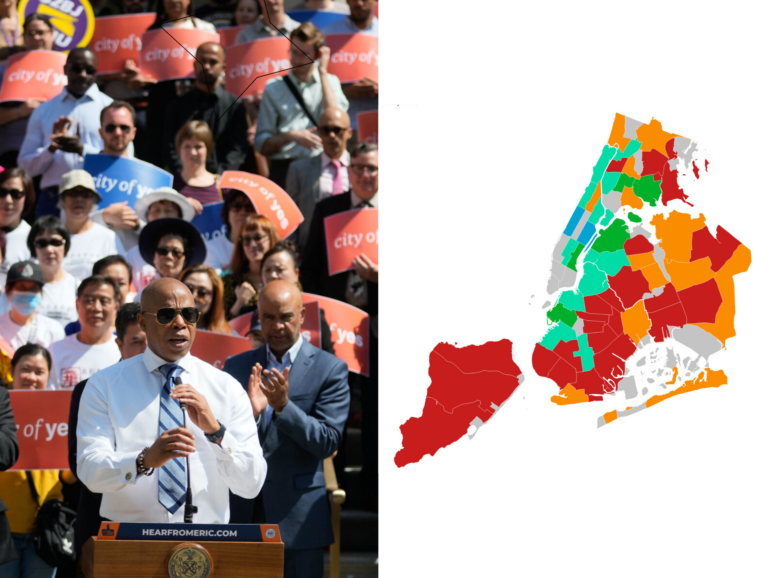
If there were no barriers to accessing the vaccine, then there would be no need to be creative in reaching people of color, Native Americans, African Americans, or immigrant communities, advocates say.

Adi Talwar
Rosa Maria Silva, 66, at Community Healthcare Network’s Sutphin Boulevard Center in Queens. Silva gave up her vaccine appointment so her 90 year old mother in-law could be vaccinated.This article originally appeared in Spanish.
Lea la versión en español aquí
Rosa Silva is 66 years old, and after a frustrating week searching for an appointment online to get vaccinated, she decided on March 6 to get on the waiting list and bide her time at Community Healthcare Network, the community health center in Queens that serves her and her husband, Edison Silva, to whom she has been married for 40 years.
That particular Saturday, the Community Healthcare Network location on Sutphin Boulevard in Jamaica had transformed itself into a vaccination-only clinic, so no other services were being provided. It is part of the ongoing efforts and strategies that local community health centers have developed to get more low-income New Yorkers and people of color vaccinated across the city.
“What we find useful,” explains Robert Hayes, Community Healthcare Network’s CEO, “is to move vaccination to churches on weekends, build a degree of trust that, combined with trust in community health centers, helps.”
Preliminary data show a disparity of vaccination among people of color, and both the city and state have launched efforts to ensure greater equity in vaccine distribution and to better reach vulnerable populations. But a budget cut by Gov. Andrew Cuomo’s administration could dent the community health centers’ funding and slow down these vaccine rollout efforts.
A lucky day
Rosa didn’t know there was that type of vaccination outreach underway at the health center a few blocks from her house. She just went there, asked how to get a shot and was added to the waiting list, on the chance that some of the people who had appointments at the center that day failed to show up. “After a while they told me, ‘We have two spots. Call your husband,’” Rosa says.
She called her husband, who arrived with Elsa, her mother-in-law, with whom the couple has been living since the pandemic began. “She [Elsa] lived alone in Brooklyn and we couldn’t leave her there in the middle of this,” says Rosa.
At 11:30 in the morning, two people had not shown up for their appointments and Rosa thought it would be best to give the vaccination slot to her mother-in-law, who in the next few days would turn 90 years old. A good birthday present, she thought.
Around noon, Elsa and Edison got their shots. Outside, in a waiting room between the vaccination area and the main hall, Rosa talked about how the pandemic had changed her life.
“I used to work from Monday to Friday cleaning offices. I had my own schedule, my own clients. I was independent, you know. Now I work one day or half a day a week. All my clients left the city. Some came back this year and I’m working with them again,” she says, sitting down as she waits to take the appointment of a third no-show. Rosa was later able to secure a spot, and was vaccinated that same day.
Resources—at a distance—for Native American NYers
Not everyone has Rosa’s luck. And the problems facing some populations have received very little attention. If you are indigenous in New York, for example, you might also face challenges with accessibility to the vaccine.
Darby Galligher, 24, is a member of the Miami Tribe of Oklahoma and is pursuing a master’s degree in public health. Under New York state guidelines Galligher is not eligible for the vaccine, but she would be eligible at an Indian Health Service facility.
The IHS doesn’t just serve people living on rural reservations out West. “One in four urban Indians live in an Indian Health Service (IHS) area,” says Ariel Richer, director of research and advocacy for the Urban Indigenous Collective. There are three IHS facilities in New York State—in Lewiston, Lockport and Manlius—but none particularly close to New York City, where 46 percent of the Native Americans and Alaskan Islanders in New York State live.
“I talked to [IHS], had to do some registration,” says Galligher, who is also the Urban Indigenous Collective’s project manager. She explains that there is no online system for scheduling a vaccination and one must call. After several weeks of waiting, her appointment was scheduled for March 28 at the Mashpee Wampanoag IHS in Massachusetts, more than four hours from New York.
“New York City,” which Galligher says is home to more than 100,000 American Indians and Alaska Natives (alone or in combination with one or more races), “does not have an IHS.”
Budget cut looms
For New Yorkers in low-income communities, community health centers play an important role in getting residents access to decent health care.
Both community health centers (CHC) and health centers that receive funds from the U.S. Health Resources and Services Administration’s Health Center Program (known as federal qualified health centers, or FQHCs) are calling for the reversal of proposed budget changes known as New York State Medicaid Carve-Out.
Under the proposed change to the 340B drug pricing program, health care providers would no longer be able to receive market-rate reimbursements for drugs purchased directly from a pharmaceutical company, an arrangement that allows them to stretch scarce federal resources to reach patients and provide more comprehensive services.
The state Department of Health argues that the change would bring about $87 million in savings, provide bargaining power through centralization, and would introduce visibility into prescription drug costs. On the other hand, community centers say they would lose operating budget funds.
The community health center where Rosa was vaccinated would lose between $5 and $8 million a year if the change were approved. “That’s 10 percent of our budget,” says Hayes.
Other community health centers, such as Housing Works, use part of those funds to build and strengthen relationships with the community they serve, says Jaron Benjamin, vice president of community mobilization advocacy for the organization.
A vital vaccine link
For Benjamin, it is contradictory that the health department would send a letter in February 2021 in which it recognizes the importance of health centers in vaccinating people of color, but has planned a budget carve-out for these centers that could begin in May 2021.
“New York State began COVID vaccinations with the counsel of a Vaccine Equity Task Force. We quickly learned that we needed to take intentional and culturally responsive steps to reach BIPOC New Yorkers. One approach to this is partnering with community health centers, Federal Emergency Management Agency (FEMA) and others to open mass vaccination sites in BIPOC communities,” read the letter from the Department of Health.
Jacquelyn Kilmer, Harlem United Community Center’s executive director, explains that the time and work her medical staff spends in vaccine outreach — educating and calling patients, listening to their concerns and fears, and fighting the stigma around the vaccine — is not billable. “The 340B [program] helps us cover the operating cost of the time we actually spend on making the vaccine successful.”
According to Kilmer, Harlem United would lose between $1.5 and $2 million annually if the change is approved. Like many other community health center leaders in the city, she believes that “it’s really the community health centers who can make this vaccine program successful. The state needs us to make this successful.”
The Community Health Care Association of New York State conducted a statewide virtual advocacy week earlier this month to criticize the proposed changes to the 340B drug pricing program.
Data and distrust
If there were no barriers to accessing the vaccine, then there would be no need to be creative in reaching people of color, Native Americans, African Americans, or immigrant communities, advocates say.
Benjamin believes the problem of the low-vaccination rate in communities of color is not a problem of distrust or hesitancy, but a problem of access. Contrary to the state’s proposed budget cut, community centers would like to receive more funding to double the number of people who are able to get vaccinated at these centers.
To get a clearer picture of who has been vaccinated in the city, advocates like Anthony Feliciano, director of the Commission on the Public’s Health System and a member of the People Of Color Health Justice Campaign, are calling for more information on race and ethnicity to be included in vaccination data. They want the government to collect data for a wider range of specific demographic groups, rather than relying on “catch-all” categories like Asian American.
“If we do not know who is sick or who is unvaccinated, we cannot target and tailor the interventions to those most at risk and facing disparities,” Feliciano says.
Without this information, Feliciano says during a press conference, it’s as if vaccination data are colorblind.