Adine Usher was diagnosed with breast cancer. She felt upset and worried. Following her surgery, when she had to find a cancer specialist, she learned about a doctor who was conducting a study using the newest cancer medicines.
The doctor she found enrolled her in a clinical trial. Now healthy and doing well, she credits the trial with having saved her life.
“If we expect the medical community to do the best by us then we should understand that can only happen if we participate in clinical trials,” says Usher, who works as an educational consultant. “I would encourage everyone on the face of the earth to try to get involved in a clinical trial,” she says.
Yet too many people in vulnerable and ethnic populations have not done what Usher did.
“In general, African-American and Hispanic/Latino men and women are currently underrepresented in most clinical trials,” her cancer doctor, Joseph Sparano, points out. He is vice chair of medical oncology at Montefiore/Einstein Center for Cancer Care, and associate director of clinical research at the Albert Einstein Cancer Center.
Clinical trials have proven to be the best way to move forward knowledge of treating diseases, and “particularly of what people in your ethnic or racial group might benefit from,” Sparano explains.
The problem is not new. A study published in the Journal of the American Medical Association looked at breast, colorectal, lung, and prostate cancer trials sponsored by the National Cancer Institute from2000 through 2002. The authors found enrollment in cancer trials to be low for all groups of patients. But “racial and ethnic minorities, women, and the elderly were less likely to enroll than were Whites, men, and younger patients, respectively.” Further, “The proportion of trial participants who are black has declined in recent years,” the study authors wrote.
Sadly, there has not been much recent improvement. A 2014 article in the journal Cancer states that while legislation in 1993 “mandated the appropriate inclusion of minorities in all NIH-funded research … twenty years after this act, the proportion of minority patients enrolled in cancer clinical trials remains persistently low.”
A clinical trial is a medical experiment that can offer patients the very newest approaches to disease cure and management. Many illnesses are now being studied in clinical trials, including heart disease, diabetes, kidney disease, asthma, Parkinson and glaucoma.
Some trials look at how well doctors and patients communicate with one another. Some look at the sleep quality of cancer survivors. Some gather information on the quality of life of people who have survived a first-time heart attack. Anything a researcher thinks should be studied and for which a rationale can be presented and funding secured might appear in a clinical trial.
Much of the reason people live longer than did people 50 years ago is because of what has been learned thanks to all the people who have participated in clinical trials.
Diversity’s medical value
Participating in a trial offers “incredible opportunities and great hope,” explains Gary Schwartz, a doctor who heads the Hematology/Oncology Division at Columbia University’s Herbert Irving Comprehensive Cancer Center, where he is deputy director. They provide “exceptional care and access to medicines that may become the standard of care of tomorrow.”
“We have to make clear to the community that we are providing opportunities to receive therapies that are not ordinarily available,” Schwartz says. And, he adds, the level of cared furnished to someone in a trial is usually of a very high level.
Why do doctors and researchers want information on, say, people whose relatives once lived in the Dominican Republic? One reason is that not all findings from studies of general populations apply equally to minority groups. For example, some medications used to control asthma were approved on the basis of studies that included relatively few Puerto Ricans and Blacks, according to Eliseo Pérez-Stable, a physician who directs the National Institute on Minority Health and Health Disparities (NIMHD). But “these are the people who have the highest rate and greatest severity of asthma,” Pérez-Stable says. What that means is that some of the asthma medicines that should be prescribed for a general population are not ideal for Puerto Ricans and Blacks.
Pérez-Stable points out that Blacks who smoke have two or three times greater chance of developing lung cancer than Whites or Latinos who smoke. Diabetes also manifests differently in different populations. Whites are more likely than others to develop heart attacks while twice as many people of color end up on dialysis.
“Clinical trials of diabetes medication should include Mexican-Americans and Puerto Ricans—populations with high rates of diabetes,” Pérez-Stable argues. “Prostate cancer trials would be remiss if they fail to enroll African-American men, who are twice as likely as White men to be affected by and die from the disease.”
Findings from large U.S. and UK trials formed the basis for current guidelines on screening for prostate cancer (specifically, measuring prostate-specific antigen or PSA). Those trials enrolled “very few African Americans,” explained Rina Das at the National Institute of Minority Health and Health Disparities. Yet Black men are twice as likely to die from prostate cancer as men in the general U.S. population, she says. So, it would be good to have more data applying specifically to the people who most need to catch prostate disease early on.
“We know African Americans are at elevated risk of developing Alzheimer’s Disease, so a plan should be in place to enroll and retain this population” from early in a study’s development, adds Carl Hill, director of the National Institute on Aging Office of Special Populations.
“Starting at the earliest planning stages of a clinical trial, it is important to think about the inclusion of disproportionately affected populations,” Hill says
Health can be affected by things that may not even usually be thought of in relation to health, and some of these may affect non-White populations disproportionately. Even something like frequency of utility outages might be relevant: Some medicines need to be refrigerated.
Recent research has identified some of the effects of experiencing racism on a person. “One important area is how chronic stress, even at a relatively undramatic level, can damage health; and how both poverty and racism are sources of chronic stress,” says Paula Braveman, professor of family and community medicine and director of the Center on Social Disparities in Health at the University of California, San Francisco. “Understanding how stress, poverty, and racism are linked is key.”
Mistrust rooted in history
Long before she herself was diagnosed with cancer, Usher was involved as a volunteer encouraging people to be screened for breast or prostate cancer, and for high blood pressure. She found much pessimism, particularly among people of color, largely because most of the people they knew who had been diagnosed with cancer had died. But that was because of late diagnosis, she says.
“The horrible mistakes of the past make many of us mistrusting,” Usher says.
“Research abuses like the Tuskegee Syphilis Experiment, which began in 1932, before safeguards were in place, will not happen again,” reads literature produced by the federal government’s National Institutes of Health. Today, all researchers are required to monitor and attempt to make sure that every participant in a clinical trial is safe. These safeguards are an essential part of the research. All researchers are required to follow strict rules designed to make sure that participants are safe. Congress has passed wave after wave of laws aimed at safeguarding the health of everyone who enrolls in a clinical trial.
“Now studies are carefully scrutinized before anyone is asked to enroll,” Sparano says. For example, if the National Cancer Institute is sponsoring the study there is “extensive review both scientific merit and to ensure that the rights and interests of people are protected.”
Get the best of City Limits news in your inbox.
Select any of our free weekly newsletters and stay informed on the latest policy-focused, independent news.
As a consequence of the laws passed by Congress and of requirements of the Food and Drug Administration, clinical trials must be registered. They must be reviewed for ethical approach and patient safety. Each clinical trial also follows a careful study plan, called a “protocol,” that describes what the researchers will do. The head researcher assumes responsibility and that researcher’s reputation is at stake in ensuring the protocol is followed.
In addition, doctors, scientists and community members at each study site must inspect the study and ensure nobody is exposed to unnecessary risks. This group of people, called an Institutional Review Board, must be in place at each study site.
Beyond that, many clinical trials are supervised by a set of experts functioning as a Data and Safety Monitoring Committee. If these experts find the treatment is not effective or is causing harm, they have the power to stop the trial.
A lack of will, or an absence of welcome?
Research indicates that, despite their misgivings, Blacks, Latinos and Asians are willing to join trials.
A 2006 study in PLoS Medicine looked at information on 70,000 individuals for a broad range of research, from interviews to drug treatment to surgical trials. The researchers concluded that “racial and ethnic minorities in the U.S. are as willing as non-Hispanic Whites to participate in health research.” The focus of attempts to correct the underrepresentation of minorities in clinical trials should not be on changing minority attitudes, but rather should be on “ensuring access to health research for all groups.”
This suggests the problem is not one of will, but one of welcoming.
Medical centers and hospitals participating in clinical trials should be going out of their way to prove to local communities that they can be trusted. “It is not sufficient for an institution to say, ‘Trust me. I will respect you.’ The first thing is for institutions to do things for the community and not ask for anything in return,” explains Nathan Stinson, Jr., director of the division of scientific programs at the National Institute on Minority Health and Health Disparities. “Organizations shouldn’t be going out into the community – organizations should already be part of the community. That’s the part that is often missing. But now some institutions ask people to participate in research or come to the organization’s clinic for care before they have demonstrated that they really are trustworthy.”
Usher warns that there are physicians who will underestimate the character of people from minority groups. “There are physicians who automatically assume this patient is not sophisticated enough to follow through with a clinical trial. That’s where racist attitudes can come into play.”
A 2014 study in the Journal of the American Board of Family Medicine involving 543 family and internal medicine physicians concluded these doctors “displayed a strong implicit preference for Whites over Blacks;” “associated ‘medically cooperative’ with Whites over Blacks;” and “reported significantly greater liking for Whites over blacks.” Yet, the medical recommendations the doctors provided did not differ for Blacks or Whites.
Similarly, a 2017 study in Academic Emergency Medicine reviewed an extensive medical literature and concluded that “although many physicians, regardless of specialty, demonstrate an implicit preference for White people, this bias does not appear to impact their clinical decision making.”
Unsurprisingly, not all studies come to the conclusion that everything that goes on in medicine is absolutely fair. For example, a 2018 study in the American College of Cardiology’s publication JACC Heart Failure looked at 104,835 patients admitted to 497 different hospitals over the course of several years and diagnosed with the very serious disease called heart failure. The authors concluded that Blacks hospitalized for heart failure are less likely than White patients to see a cardiologist.
The question of risk
Almost all things medical involve some risk. Medicines carry side effects. Surgeries can have complications. Cardiovascular exercise like running is good for your heart but, if you haven’t the perfect stride, can be tough on knees, hips and backs. The only way to avoid medical risk is to stay healthy.
What risks might be involved if you are in a clinical trial? The National Institute of Health spells some of these out. Patients cannot be afraid to ask questions: Will the trial inconvenience me, for example, by taking a bunch of my time? Is it possible the new treatment may not work? Might the new treatment prove to be no better than standard treatment? What if I do not receive the new treatment? Might the side effects be worse than those of current standard treatments? What are the worst adverse events that might occur? How do the problems I might have if I go into the clinical trial compare with the problems I might have if I do not enter a trial? Might I die?
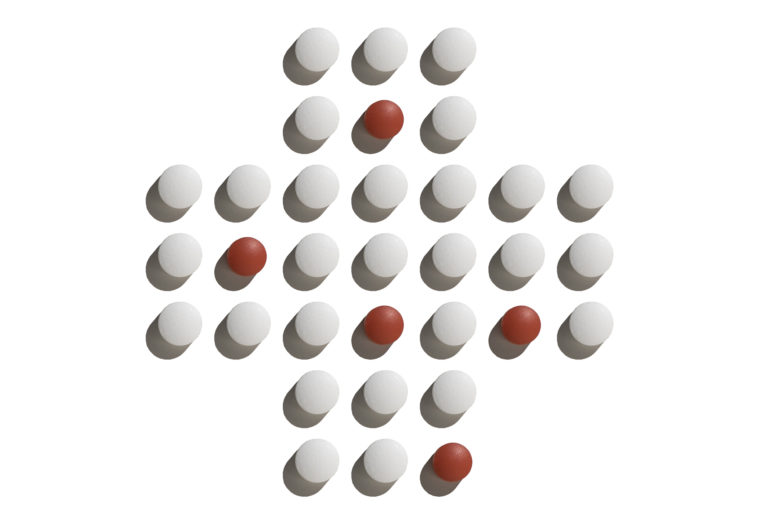
Many clinical trials explore a new treatment or new medicine by comparing the new approach with the standard of care, that is, with the recommended way most patients should be treated. Some clinical trials use something called a “placebo.” A placebo appears to be a treatment or medicine but, in fact, has no active ingredient. So, for example, someone with insomnia might enter a placebo-controlled trial in which two-thirds of patients receive a new medicine while one third receive a placebo. Using a placebo in this way helps scientists differentiate between effects of the new medicine itself and effects connected to the excitement of being in a medical study.
Health Disparities
•NY Support Lags for Sickle-Cell Patients Facing Pain, Poor Treatment, Discrimination
•Death’s Disparities: Health Inequality in New York City
Some areas of medicine are less likely than sleep medicine to use a placebo in this way. In testing a new cancer medicine where a combination of three drugs are known to benefit many patients, for example, it would be wrong to stop treatments known to help people. As the American Cancer Society says, “It’s unethical to give someone a placebo if it would deny the person a chance to get a drug that’s known to work.” Reinforcing this message, the American Society of Clinical Oncology – the official organization of cancer doctors – says, “You will never get only the placebo.”
As the U.S. National Cancer Institute says, “Placebos are rarely used in cancer treatment clinical trials.” There are clinical studies in cancer medicine in which some patients receive the three proven drugs plus a new medicine while other patients receive the three proven drugs plus a placebo. In such a study even the people receiving the placebo gain the benefit of proven medicines. Plus, in the rare instances in which a cancer clinical trial uses a placebo, you will be informed about that in advance. And you never, ever are forced to go into a clinical trial if you do not want to do so. Meanwhile the extra attention and special care that goes with being in a clinical trial goes to all of the patients.
“Patients have to understand everything about the trial,” Schwartz says. There must be complete honesty about the risks and benefits. Everything should be explained without fancy scientific terms, as far as possible. The explanation should be culturally appropriate for the individual patient, he says, and this should include complete translation, where needed.
A local focus
The National Cancer Institute has designated as “minority/underserved community research sites” two hospitals in New York City — Dr. Schwartz’s Columbia and Dr. Sparano’s Montefiore Einstein.
According to the National Cancer Institute, these sites have patient populations comprised of at least 30 percent racial/ethnic minorities or rural residents. The sites focus on cancer prevention, control, screening and post-treatment surveillance clinical trials, as well as treatment, imaging and quality-of-life trials.
At the same time, many other New York hospitals are very actively involved in conducting clinical trials. Some clinical trials currently being conducted here include the following:
In the Bronx, the Montefiore Medical Center and the University Hospital for the Albert Einstein College of Medicine are now conducting a study enrolling Latino and Black adolescents with asthma, ages 10-17 years old, and their caregivers. Adolescents and caregivers will work together with a coach to learn about asthma and behavioral strategies to improve their asthma control. The goal is to improve adolescents’ abilities to recognize when asthma symptoms occur and ways to avoid asthma triggers. This may reduce the frequency of rushing adolescents to the emergency department.
In Northern Manhattan, the Columbia University Medical Center is conducting a study of Alzheimer Disease in Caribbean-Hispanic Families. The study seeks to identify genes that may increase the risk for developing Alzheimer’s. The study will enroll families and/or individual who are 60 years of age or older, both those with and those without memory problems.
In Northern Manhattan and the Bronx, both the Columbia University Medical Center and the Montefiore Medical Center are participating in a clinical trial investigating why certain racial and ethnic populations are at increased risk of developing cancer at an early age. African-American, Hispanic, Native American, and White patients with breast, prostate, colorectal, and liver cancer as well as a specific cancer of White blood cells (multiple myeloma) may enroll. Researchers will record genomic data as well as data regarding patients’ demographics, histories, treatments, responses, and outcomes. This trial seeks insights into the biology of early disease, tumor progression, and treatment response.
The findings might possess the potential to uncover molecular targets and biomarkers for prevention, early detection, treatment, and disease monitoring.








2 thoughts on “In NYC and Around the Country, Racial Skew Hampers Trials for New Medicines and Treatments”
Pingback: In NYC and Around the Country, Racial Skew Hampers Trials for New Medicines and Treatments – City Limits | Minority Health
Pingback: Company Updates: February 2019 – Recruitment Partners