Adi Talwar
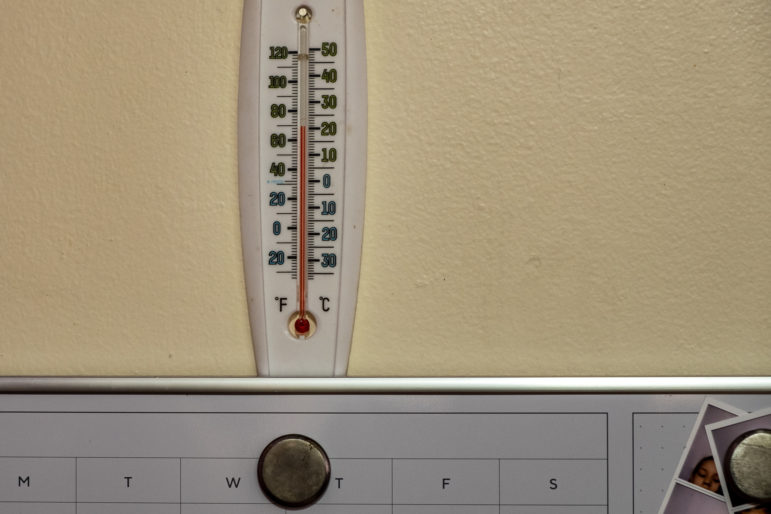
The formula display inside a Key Food Supermarket on Jerome Avenue near Gun Hill Road in the Bronx.
Each day, dozens of mothers – with babies on their laps – sit inside a lounge at Bedford-Stuyvesant’s Woodhull Hospital where peer counselors and nutritionists from the Food for Women, Infants and Children (WIC) program help guide them through parenting’s many trials. Behind the families, small framed posters display facts about breastfeeding, evidence of WIC’s role in a broad national, state and city effort to increase breastfeeding rates, especially among low-income families.
“There is a misconception that modern mothers don’t breastfeed,” reads one sign behind a woman with a nursing cover draped across her torso. The woman warmly greets a staff member before lifting her baby and walking to a quiet office area. Other posters describe the health benefits of infant breastfeeding, which is associated with a lower risk for gastrointestinal disorders, respiratory ailments and type 2 diabetes than in babies who do not breastfeed.
Though breastfeeding rates are up statewide – from 62 percent of new mothers in 2002 to 82.4 percent in 2014, according to the New York State Department of Health (NYSDOH) – only a tiny proportion of new mothers breastfeed without using formula in many of New York City’s low-income communities, like the area around Woodhull.
Just 1 percent of mothers in Brownsville and 3 percent in Bedford-Stuyvesant breastfeed exclusively for six months, the city’s Center for Health Equity reports.
Advocates and mothers say that more one-to-one outreach – like the WIC peer counselor program – can successfully overcome the social alienation, cultural assumptions and even workplace obstacles that prevent women from continuing to nurse their infants.
How WIC and NYC promote breastfeeding
To many New Yorkers, ‘WIC Accepted’ posters on glass bodega doors portray the program as nothing but a supplement to a family’s food budget, akin to Food Stamps. WIC, however, also provides comprehensive services to new mothers and their children for up to five years.
Each month, WIC gives participating families monthly paper checks worth about $70 to purchase food and baby formula that meet FDA nutrition guidelines. Families also receive vouchers worth up to $15 per month to purchase fruits and vegetables.
New York’s WIC program approves four types of formula by two manufacturers – Enfamil and Gerber – that bid for WIC contracts. After receiving medical approval, families can purchase several other specialized formulas for premature infants, babies with allergies and other health considerations.
The state reimburses the bodegas, supermarkets and other businesses that enroll as WIC vendors and accept the monthly checks from customers. The New York State Department of Health contracts with 92 community-based organizations that run WIC programs at 400 clinics statewide and serve at least 50 percent of infants born in the state each year.
To qualify, a woman must be pregnant, have a baby less than six months old or have a breastfeeding baby less than a year old. She must also receive Food Stamps, Medicaid or public assistance or meet federal income requirements – no more than $37,777 for a family of three. Children under five whose families meet income requirements also qualify. Immigration status does not affect participation.
The United States Department of Agriculture funds nearly 98 percent of New York’s WIC program and the state pays the remainder.
While WIC has long promoted breastfeeding among its participants, the federal government empowered WIC to play a bigger role in promoting nursing through a peer-counseling program that began in 2004. Based on the program’s success, the Surgeon General in 2011 recommended that each WIC program employ peer counselors – former WIC participants with their own breastfeeding experience – to connect with, educate and encourage new mothers as they try to consistently nurse their young children.
Each local WIC office hires its own counselors who contact every woman enrolled in the program and try to meet with new mothers a few days after birth. Counselors are available to talk or meet outside office hours, which further helps develop rapport and trust, says Woodhull WIC breastfeeding coordinator Felicita Anton.
“The mothers feel so confident with their peer counselors that [after delivery] they say, ‘Can you come up and help me position the baby?” and they go because they don’t want to lose that trust,” Anton says. “[The counselors] are the first hand-to-hand connection and that opens up a bridge.”
Despite the state and federal government’s acknowledgement of the key role peer counselors play in promoting breastfeeding in low-income communities, individual counselors in New York City manage caseloads of hundreds of families.
The Woodhull WIC program employs two peer counselors who serve between 400 and 500 families, Anton says. At some sites in the Bronx, each counselor works with about 150 families, though few mothers continue breastfeeding and meeting with their peer counselor for the recommended six months, one peer counselor says.
In addition to empathy and emotional encouragement, counselors provide practical guidance – like methods for holding a baby and expectations for how much milk a mother will produce – share information about public breastfeeding protections and troubleshoot specific nursing problems as they arise.
When one discouraged woman told her counselor that breastfeeding irritated her nipples, the counselor asked her to remove her shirt and showed her how to cover her own nipple with the nipple from a baby bottle. The barrier worked to relieve the pain and the woman continued nursing.
Yet, one new mother who works in social service says the emphasis on breastfeeding can be overwhelming and make women who feed with formula feel like failures. She says she put pressure on herself to exclusively breastfeed but struggled until a friend gave her formula coupons and suggested she share her anxiety with her baby’s pediatrician. The woman says she felt relieved when the doctor then encouraged her to mix breastfeeding and formula use. Medical experts recommend mothers talk with their health professionals about such anxieties and say mixed-feeding still provides the immune-system and infant-mother bonding benefits of breastfeeding.
Such experiences are common among mothers who commit to nursing. Anton says she encourages all mothers to breastfeed but wants each person to pursue the experience that works best for her and her infant.
“It about personal choice,” Anton says.
City support for new moms
Over the past decade, New York City has significantly increased efforts to promote breastfeeding by recruiting hospitals, healthcare providers and nonprofit agencies in the mission.
In 2007, the city’s Health and Hospitals Corporation (HHC) banned formula manufacturers’ coupons and samples at its facilities and in 2012, the city enlisted private hospitals to voluntarily limit formula marketing as part of its Latch On initiative.
Seven HHC facilities – as well as eight others in New York City – have received a Baby-Friendly Designation based on standards for breastfeeding education and mother-baby bonding outlined by the World Health Organization and Unicef. Woodhull, the first Baby-Friendly Designated hospital in Brooklyn, has undergone significant changes in how it engages new mothers, says head of midwifery Helena Grant, who has worked at Woodhull as a nurse and midwife for more than twenty years.
“Doctors are very involved with patients by encouraging breastfeeding, nurses are getting into it,” Grant says. “We are holding women in [their] space of power and telling them, ‘We’re here to support to you.’ It’s a holistic experience.”
The City Council passed a law last year mandating lactation spaces at all city agency sites that provide social services. The Breastfeeding Empowerment Zone (BFEZ), a Center for Health Equity program based in Brownsville, also helped develop 89 lactation spaces throughout Bedford Stuyvesant and Brownsville, including inside grocery stores, libraries, restaurants and laundromats. In August, the city opened a lactation pod in each borough – including at the Brooklyn Children’s Museum – for mothers to breastfeed in private.
“We envision a city where children have the full opportunity to grow up healthy regardless of where they live. Our goal is to create communities where breastfeeding families receive consistent support in the hospital, at home and at work. To attain this goal, a cultural shift is required. We will continue our efforts to address breastfeeding disparities and to foster a breastfeeding friendly culture citywide,” the city’s Department of Health and Mental Hygiene said in a statement to City Limits.
According to city data derived from birth certificate information, the Office of Vital Statistics and the Pregnancy Risk Assessment Monitoring System (PRAMS), 92.2 percent of infants citywide breastfed in the hospital in 2015, including 92.4 percent of infants in Bedford Stuyvesant and 91.7 percent in Brownsville. Greenwich Village has the highest percentage of infants who breastfeed at the hospital – 98 percent – while Tottenville in Staten Island has the lowest – 76 percent.
Meanwhile, the BFEZ website says 88.2 percent of New York City mothers initiate breastfeeding but only 29.6 percent exclusively breastfeed for at least eight weeks.
In a study published in the July issue of the journal Pediatrics, researchers who studied the breastfeeding and formula supplementation rate of all infants born in New York state in 2014 found that 26 percent of breastfeeding infants also received formula in the first two days after birth compared to the national average of 17 percent.
The study indicates that infants born to Black, Hispanic or Asian-American mothers and mothers with insurance through Medicaid were more likely to receive formula supplementation than those born to white mothers, but the rates varied widely across hospitals.
Structural barriers to nursing for low-wage workers
Despite the effort to support new mothers with lactation spaces at businesses and public spaces, many low-wage workers who begin breastfeeding face obstacles when they return to work, Grant says.
“It’s a mental act of might to continue breastfeeding in the work environment,” Grant says, adding that accommodations for women in office settings typically do not apply to women in low-wage work settings, like bodega clerks or shoe store employees. “There may be a backroom that is a stockroom. There is not the luxury of a calm space.”
Mothers who work as home health aides – one of New York City’s fastest growing industries – face unique challenges to expressing breast milk because they work in other people’s homes, including tiny studios or single-room occupancy apartments with shared hallway bathrooms.
One former home health aide who now works as a security guard says the decision to breastfeed depends on the relationship with the individual patient. She also says women in her native Trinidad feel much more comfortable breastfeeding in public than in the United States where they consider formula use “the American way.”
Another home health aide – a mother of three from the Dominican Republic who lives in Bedford Stuyvesant – says she felt supported by the homecare agencies she has worked for because they allowed her to set her schedule based on her family’s needs. In the Dominican Republic, she says, formula is expensive and viewed as a luxury while in the United States, formula is expected and more easily obtained through WIC, food stamps or manufacturers’ coupons.
Several home health care agencies did not respond to request for information about their accommodations for new mothers, but a spokesperson for Visiting Nurse Service of New York (VNSNY) replied by email. VNSNY runs Partners in Care, one of the city’s largest home health care providers.
“Upon request, we will adjust the HHA’s schedule providing flexible hours as suits her schedule,” the spokesperson wrote, adding that Partners in Care will also provide private office space for mothers to express breast milk. She did not directly address the challenge home health aides would face by leaving their patients and traveling to the office.
“When requested, an HHA’s client hours will be adjusted to accommodate her personal needs. If that means sending in another aide to cover for her, then that’s what we do,” she added. “In some cases clients are happy to provide privacy for an aide in the home, but that is handled on an individual basis.”
A home health aide who works for Partners in Care says that what some might consider flexibility, she considers instability and a challenge for new mothers. An aide’s three-hour shift could become an eight-hour shift if a doctor prescribes additional homecare for a patient. The agency can also abruptly transfer aides based on a patient’s request or agency need.
Meanwhile, a fourth aide says she considers breastfeeding in public “a little disgusting” and that she would not pump breastmilk on the job or anywhere else except the privacy of her home.
Anton, the Woodhull breastfeeding coordinator, says restaurant, factory and hotel jobs are also challenging environments for expressing breast milk. She and a peer counselor worked with one hotel maid who wanted to continue nursing after she returned to work, where she remained on her feet, moving among hotel rooms throughout her shift. The peer counselor guided the maid by helping her gradually adjust her baby’s nursing schedule and showed her how to express and dispose milk into hotel bathroom sinks, which relieves pain related to engorgement while ensuring continued breastmilk production.
The high cost of formula
Breastmilk may be free nutrition, but formula is often a more convenient option – especially for working mothers. Thus, plenty of local businesses compete for the newborn market, stacking pallets of powdered formula securely behind their counters.
Families feeding infants with formula can choose from several stores along the Webster Avenue corridor through Claremont and Morrisania, which features a dense concentration of public housing towers. Of 23 small stores – 22 bodegas and one pharmacy – seven did not sell formula, though clerks at two stores said they were awaiting new shipments. All sixteen stores that did sell formula stocked Enfamil brand – what one clerk called “the regular kind” – typically in 12.5 oz. tubs of powder at an average price of $19.39. While one African market sold the container for $17, all other stores priced their formula between $18.99 and $20. One bodega sold a 27.5 oz. tub of powder formula for $40. Five stores sold cans of liquid Enfamil formula – which have a shorter shelf life and provide fewer servings – at an average price of $5.74.
Seven of the stores, including the pharmacy, accepted WIC. Four had signs advertising formula or displayed formula in their street-facing windows. Only one shop kept their formula somewhere other than behind the counter.
At a Food Bazaar near Crotona Park an employee stood next to shelves stocked with an array of formulas with green “WIC Approved” stickers next to the price tags. The supermarket formula costs about the same as the formula at the bodegas, but Food Bazaar customers with IDNYC cards can save 5 percent on their total purchase.
Amazon sells 12.5 oz containers of powdered Enfamil Infant formula for $16.99.
Yet, to one shopkeeper in Highbridge, the city’s efforts to encourage breastfeeding may be paying off. When asked if he sold formula, the bodega owner said he had recently stopped stocking the formula because not enough people were buying it.
CityPlate, City Limits’ series on food policy, is supported by the Laurie M. Tisch Illumination Fund. City Limits is solely responsible for the content.