Mary Marco, an elegant, soft-spoken woman, spends a lot of her time on the grounds of the Bronx Psychiatric Center, but she doesn’t have to. It’s been nearly 20 years since the keeper of the hospital’s gift shop called the wards home.
She credits her long tenure without hospitalization to the support of her sister Paulina Magnetti, with whom she lives in the Country Club section of the Bronx, as well as to the regular counseling sessions she gets at nearby Jacobi Medical Center and the medication she takes for schizophrenia.
Marco is one of thousands of New Yorkers who are able to live outside of the state’s hulking psychiatric hospitals thanks to neighborhood-based treatments and services.
In fact, it’s for the sake of those local services–as well as for reducing New York State’s $11.5 billion budget gap–that Governor Pataki has proposed closing the Bronx Psychiatric Center and Children’s Psychiatric Center and three other state-run psychiatric facilities in Middletown, Elmira and Syracuse.
“Do we continue to fund beds at the expense of community beds that are needed, or do we consolidate somewhat?” asks Roger Klingman, spokesperson for the state Office of Mental Health.
The answer, it seems, is neither.
A month before the governor announced his plans to close the five hospitals, he vetoed a bill that would have put the Community Mental Health Reinvestment Act back into effect by this July. First passed a decade ago, the law required that money saved from cutting psychiatric beds go toward counseling at Medicaid-financed clinics and small residential housing facilities.
During the law’s eight-year lifespan (it expired in 2001), the state eliminated about 5,000 psychiatric hospital beds, leaving 4,200 in the system. Local mental health service providers did see some of the savings–$212 million, according to the state comptroller’s office. But another $100 million, by some estimates, was diverted into the state’s general fund.
The law “has failed to live up to its promise,” says Joseph Glazer, president and chief executive officer of the Mental Health Association in New York State. That loss, he says, has resulted in treatment programs for the mentally ill “battling for the scraps from the table.” So why should the governor be trusted now? he asks.
Pataki’s December veto is hardly a promising sign. Explaining that he rejected the reinvestment bill because state law prohibits the legislature from determining how funding is appropriated, Pataki promised to include a new version of the law in the state budget, which as of late April was still under negotiations.
But even if the governor’s bill passes, it will not take effect until next summer, too late to ensure that at least some of the savings from the hospital closures go to neighborhood services, advocates for the mentally ill say. The three upstate hospitals are slated to shut their doors by July 1; the $16.7 million saved will go directly into the state’s general fund.
Assemblyman Peter Rivera, chair of the Assembly’s Mental Health Committee, has sponsored rival legislation that would immediately salvage that money for community services.
Still, Rivera’s top priority is keeping the Bronx facilities open, despite state budget officials’ claims that closing them would save $74 million. He says he’s received 100,000 letters and petitions from people as far away as Sweden and China who support the effort to save the hospitals.
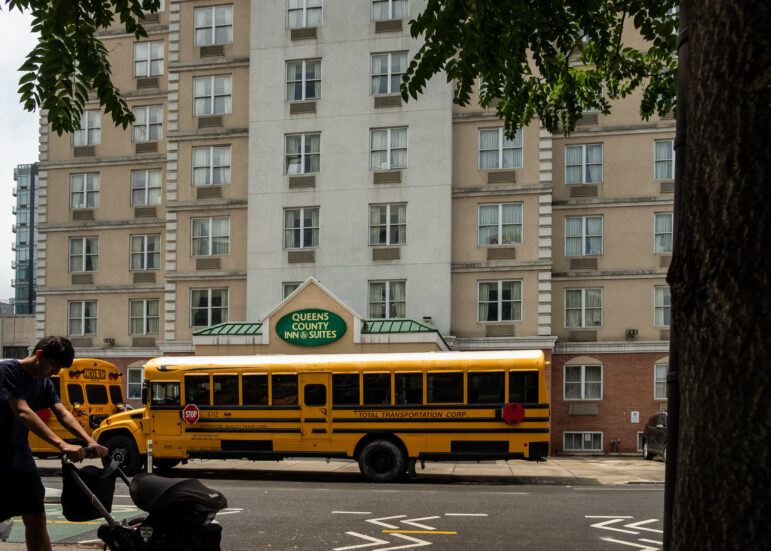
The aggrieved writers’ primary complaints: The Bronx would become the only borough without its own state psychiatric hospital, and the state would lose its only wards designed for Spanish-speakers. Moving patients to Pilgrim State Psychiatric Center in Central Islip, Long Island, and Creedmore Psychiatric Center in Queens–as Pataki proposes–would alienate them from their families. (Upstate patients would also be shifted to far-away hospitals.)
And if patients’ only options are living hours away from their families or living on the streets, they might choose the streets. “For a small percentage of people…there may be a seriously violent episode, the kind we read about in the papers and that we really shudder about,” says Dr. Robert Lowinger, a psychiatrist at the Bronx facility and an executive board member of the Public Employees Federation, which opposes the closures.
Even the Bronx’s neighborhood-based programs consider the hospital a hub of psychiatric services in the borough. Noris Colon, founder and executive director of HOGAR, a South Bronx housing program and clinic serving 27 people with psychiatric illnesses, many of whom don’t speak English, says closing the hospital would kill her program.
“If they close down,” she says, “I close down with them.”
Maura McDermott is a Bronx-based writer.