The Birth Center at Bellevue Hospital was designed for the kind of birth experience that many moms, even the well-connected, find elusive. Labor was to unfold in spacious, comfortable rooms with sweeping views of the East River; midwives would massage women through labor pains; and world-class obstetricians would be at hand to address any complications. All this in a public hospital that primarily serves low-income patients and the uninsured, many of them immigrants.
So when hospital administrators quietly shut down the 12-year-old center this September, New York’s tight-knit community of midwives and natural birth advocates demanded another look.
“It’s heartbreaking and really angering,” says Elan McAllister, founder of Choices in Childbirth, an organization that promotes low-intervention birth options in New York City. “The birth center is an incredible model that’s decreasing racial disparities in maternal care. But the people making decisions are completely uneducated about it.”
Bellevue administrators say that shrinking Medicaid reimbursements, state budget cuts and a looming $30 million budget deficit have forced them to cut costs. But midwives who worked there say that the center was undermined by the hospital’s own staff, who routinely denied patients access to the birth center.
“Women would come in for the hospital tour and they’d be absolutely thrilled to see the birth center, because it’s so beautiful in there,” says Kimm Sun, a midwife who worked at Bellevue in 2006. “It was horrible, because you knew they weren’t going to get that experience when the time came.”
A low-tech approach
The situation was different in 1998, when Bellevue’s public relations office touted the new center as a model of low-cost, high-quality care. Directly across the hall from the 12-bed labor and delivery (L&D)unit, the four birthing rooms were outfitted with Jacuzzi-style tubs, rocking chairs and spacious beds. There was ample space for visiting family and friends.
The birth center’s homey decor served a deeper purpose. Such facilities are designed to support women who are able and willing to give birth with minimal medical assistance. Modest luxuries like tubs and birthing balls replace high-tech interventions like spinal epidurals and constant fetal monitoring. While sometimes medically necessary, the widespread use of the more intrusive practices even in low-risk labors has been linked to the country’s soaring c-section rate, which increased 50 percent over the last decade.
The factors behind the increase in c-sections, from mothers’ fear of pain to physicians’ anxiety about malpractice suits, are subject to heated debate. About three out of every 10 births in the United States are by c-section; in 2007, the rate in New York State was nearly 34 percent. Compared to vaginal births, c-sections carry a higher risk of complications, a longer recovery period, and lowered immunity in the baby. They also cost insurers at least 50 percent more than normal births, according to a report from Childbirth Connection.
Like most hospitals, Bellevue has seen a steep climb in its overall c-section rate, from 18 percent of births in 2000 to 27 percent in 2007. Over the same period, the birth center maintained a c-section rate below four percent, according to unpublished figures collected by Richard Jennings, Bellevue’s director of midwifery. While the numbers are difficult to compare—by definition, women admitted to the birth center were unlikely to experience labor complications—the birth center’s consistent outcomes showed it to be a bulwark against the spreading c-section trend.
In a recent letter, Public Advocate Betsy Gotbaum questioned the Bellevue administration’s decision to close the birth center, noting that the hospital has the third-lowest c-section rate in Manhattan. In her reply, Bellevue Executive Director Lynda Curtis cited low demand as a reason for the closure. According to hospital records, the number of patients using the birth center declined from 353 in 2004 to 125 last year.
But others who worked there say that the real issue was an uncooperative staff, rather than a lack of willing mothers.
Nurses unavailable?
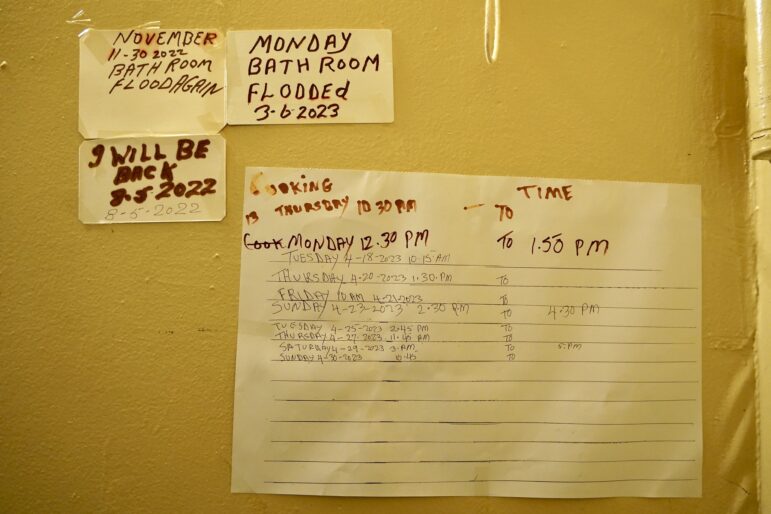
According to some midwives and volunteer birth attendants, many Bellevue nurses proved unwilling to accommodate the pace of labor in the birth center. Their participation was crucial, however, as hospital regulations require that a nurse be on hand to document and monitor every patient. Melanie Peña, a volunteer doula in 2007 and 2008, says she attended only two births there during her monthly rounds. At one point, a laboring mother and her midwife both asked to use the birth center, but were told that the nursing staff could not afford to send someone to the “other side.”
A spokeswoman for the Bellevue chapter of the New York State Nurses Association declined to comment for this article. A spokesman for Bellevue Hospital did not reply to a question about whether the hospital’s staff diverted mothers from the birth center to L&D.
For nurses, birth center procedures tend to be more time-intensive than those in standard labor and delivery rooms. Technology makes a difference: In the L&D suite, the laboring mother is hooked up to a monitor that measures her contractions and fetal heartbeat. This technology allows nurses to track the birth remotely, though it also constricts the mother to her bed. In the birth center, the mother is free to move around, and nurses check the fetal heartbeat intermittently with a handheld device. The low-tech approach requires more hands-on attention from attending nurses and midwives.
Without support from hospital staff, the birth center languished, midwives say.
Tania Luna, who was a volunteer doula in 2006, says that her Spanish-speaking patients rarely knew the birth center existed. Even those that did were not necessarily eager to use it. For some immigrant women, a high-tech hospital birth represented a slice of the American dream. Others, particularly from rural areas, were suspicious of medical procedures at odds with their own birth traditions. Whatever their preference, access to the birth center was largely a matter of luck.
Margarita Flores, 23, had already given birth twice at Bellevue before she learned of the birth center during her third pregnancy. Her midwife arranged to open the center for the birth of Flores’ daughter this August. “It was a beautiful experience,” says Flores, who is from Puebla, Mexico. “We had more privacy, a bigger room.” She adds that her nurses and midwives were kind and attentive in all three births.
Demand and supply
Although Bellevue does not plan to reopen the birth center, women can still have a low-tech, midwife-attended birth in one of the standard delivery rooms, says hospital spokesman Stephen Bohlen. The hospital will retain the midwives currently on staff. Still, supporters of the birth center doubt that women will have the same quality of experience on the L&D floor—especially given the difficulties of asserting birth preferences in the throes of labor.
Even as the Bellevue center remains under lock and key, demand for such facilities is on the rise across New York City. Attending midwives at St. Luke’s-Roosevelt Hospital keep waiting lists of mothers who want to use the hospital’s birth center. At St. Vincent’s Hospital, the planned Eli & Abby Manning Birth Center will offer acupuncture, hydrotherapy and other forms of natural birth support.
Neither center, however, is focused on the working class, immigrant-heavy population that defines Bellevue. And that leaves some angry. “If this were a population of assimilated, educated women, Bellevue would not stand a chance of closing down the birth center,” says Sun. “But these women, they’re barely making a living—they’re just happy to have a kid here.”
In the five boroughs, only two birth centers remain that accept women on Medicaid: the Brooklyn Birth Center near Coney Island, and the Morris Heights Birth Center in the Bronx.