Youth and advocates are optimistic, saying Gov. Kathy Hochul’s budget takes important steps to expand resources, but that more needs to be done to make up for years of ‘chronic underfunding’ across the system.

Adi Talwar
Madyson Oneiya, a member of the youth advocacy group Students Break the Silence, which is advocating for more mental health resources for New York City students.After graduating high school last spring, Meril Mousoom spent most of the summer quarantined in their parents’ home in Queens–the same place they’d also camped out during the remote classes that dominated the second half of their high school experience.
That summer, Mousoom was overwhelmed with suspense. After two years in quarantine, going away to college in Minnesota felt more significant, and more uncertain.
“Because we’re so young, COVID has just been like the biggest thing that we are seeing,” said Mousoom, who is 18 years old. “For us, it’s like the most defining moment of our lives.”
Like many others dealing with the pandemic’s mental health repercussions, Mousoom needed extra help. But they couldn’t find consistent, reliable behavioral health resources they could depend on.
Instead, Mousoom has had to cope with the panic disorder they developed that summer––in addition to pre-existing anxiety, depression and ADHD—mostly on their own.
Youth across the city, state and country have experienced an uptick in mental health concerns in recent years. Amanda Fialk, a partner and chief clinical officer at a Manhattan-based mental health clinic for youth called The Dorm, said she’s seen a 40 percent increase in youth anxiety since the start of the pandemic.
“Youth do not have access to timely, coordinated, and quality mental health care, which is tragic, as consistent and accessible care can transform the life of a young person struggling with mental illness,” Fialk said.
Prior to the pandemic, mental health challenges were the leading cause of disability among youth, according to the U.S. Department of Health and Human Services. Nationwide, one out of every five children between ages 3 and 17 suffered a mental, emotional, developmental or behavioral disorder. In the decade before COVID struck, feelings of sadness among youth increased 40 percent while suicidal behaviors increased 57 percent. As the pandemic exacerbated the conditions leading to these rates, the U.S. Surgeon General issued an advisory about the crisis.
“The COVID-19 pandemic further altered their experiences at home, school, and in the community, and the effect on their [youth] mental health has been devastating,” Surgeon General Dr. Viveck Murphy said in the December advisory. “The future wellbeing of our country depends on how we support and invest in the next generation.”
In her proposed $216.3 billion state budget for the upcoming fiscal year––which is over $4 billion larger than last year’s record breaking budget––Gov. Kathy Hochul plans to invest $53 million for children’s mental health services. Funds will be used to integrate behavioral health services into pediatric primary care, align Child Health Plus Benefits with Medicaid and provide more home-based crisis intervention. The governor also proposes bonuses for behavioral health workers as part of a plan to grow the workforce by 20 percent over five years. Additionally, the budget will invest in schools, with the opportunity for some of that money to go towards the expansion of school-based mental health resources.
READ MORE: How Does New York State Come Up With a Budget? We Asked the Experts
The governor and state lawmakers will hammer out the final plan in the coming months, ahead of the state’s April 1 budget deadline. Despite the record spending in Hochul’s executive proposal, some youth leaders and advocates say addressing the root causes of the youth mental health crisis requires going further, due to a deficit created by chronic underinvestment.
“While we’re taking really important steps forward with Governor Hochul, there’s also such a great need,” said Alice Bufkin, the associate executive director for policy and advocacy at Citizens Committee for Children (disclosure: CCC is a City Limits’ funder). “This is a system that has been chronically underfunded for years and years and years. We’re essentially starting at a deficit that is very large in terms of where we are investing in children and where we need.”
Easier, earlier intervention
The budget includes $10 million to expand HealthySteps, a program where a developmental specialist is fully integrated into pediatric primary care to intervene with families of children up to 5 years old, according to Cort Ruddy, deputy communications director for health at the governor’s office. Ruddy said there are currently 13 HealthySteps affiliated sites and the funding for FY22 is $858,330. Hochul plans to use the $10 million in FY23 to create an additional 57 sites, according to Ruddy.
Mousoom–a member of the youth advocacy organization called Students Break the Silence–thinks the effort could help expand access to kids from an earlier age, something. Mousoom says they grew up without access to many mental health resources due to structural inequities that created historical healthcare barriers for their Bengali community in Queens. Mousoom says their family only started to take mental health seriously after they were hospitalized. They wish a program like HealthySteps was implemented when they were younger so they could get help sooner.
“Especially thinking about the demographics of New York, especially New York City, I think it’ll be super helpful for people to have it early on because I wish that I had gotten diagnosed earlier, too,” Mousoom said.
Sandra Runes–the former director of psychological services, unit chief for the Child and Adolescent Psychiatry Service and chair of the ethics committee at Lincoln Medical Center, who retired in January–says HealthySteps could help families feel more comfortable seeking out mental health treatment by making it a more routine part of their care.
“Mental health always has a stigma,” Runes said. “But if [the pediatrician] says, ‘Oh, you know what, there’s another person down the hall in this third office, they’re going to see you next time, just come here,’ they come. So integrating it into primary care takes away some of the stigma that you’re not going to the crazy clinic.”
The governor also aims to expand access for children who rely on Child Health Plus––a public insurance option for kids––by aligning their benefits with Medicaid. The executive budget invests $11 million in FY23 and $44 million in FY24 for making the change.
Runes thinks this is an important step: certain benefits that kids can access through Medicaid, but not yet with Child Health Plus, can make all the difference, she says. For example, Medicaid provides MetroCards to families who need mental health services. Since mental health requires ongoing treatment, Runes says families using Child Health Plus can be discouraged by transit fees required to travel to appointments. Providing MetroCards could help some families get to the clinics they need.
The budget also includes a plan to bring more providers to patients by investing $7.5 million in the expansion of home-based crisis intervention services, which aims to provide short-term, intensive, in-home services to families with a child between 5 and 17 who is experiencing a severe psychiatric crisis. There are currently 33 home-based crisis intervention programs across the state serving roughly 1,320 families annually, according to Ruddy. The funds for FY23 will be used to develop 10 new programs, as well as increase funding to all existing programs. Ruddy said the goal is to double the amount of families served each year.
Bufkin said these often help stabilize kids after they leave the hospital––a critical juncture in their care.
“Often those transition points are particularly challenging times because if they don’t have anywhere to go back to then they don’t have the opportunity to get the support,” Bufkin said. “We don’t want to continue the cycle of children needing to turn to hospitals for the supports they need.”
Workforce shortage
Mousoom depends on the nurse at their college to prescribe their medications, as they’ve been unable to find a therapist that’s been willing to accept them as a consistent patient.
“Every single time that I call an office––like I’ve been calling the office for months and months––they’re either saying that ‘we don’t have enough staff’ or like ‘we don’t have openings at the moment’ or they just don’t respond,” Mousoom said.
Fialk said outpatient programs––behavioral health services provided outside of hospitals––are facing a major workforce shortage that cannot keep up with the youth demand.
“Outpatient programs are plagued by long waitlists and a shortage of providers,” Fialk said. “We desperately need more community-based mental health and recovery services and support, so kids can access care and avoid the revolving door of emergency room ‘treatment’ for mental health concerns.”
Bufkin said the shortage is caused by inadequate pay, which stems from low reimbursement rates that behavioral health providers receive from health insurance providers.
“A lot of that does relate to chronic underinvestment in the rates for providers,” Bufkin said. “And that’s true both in public health insurance, like Medicaid, and it’s also true in commercial insurance, which tend to have deeply inadequate rates.”
As part of Gov. Hochul’s plan to grow the healthcare workforce by 20 percent over the next five years, the executive budget includes over $200 million in state resources to fund bonuses for frontline, direct care and clinical workers in the mental hygiene sector, according Ruddy. The executive budget also includes a 5.4 percent cost-of-living adjustment to human services providers in FY 2023 so providers can offer more competitive wages to their staff, Ruddy said.
New York’s behavioral health workforce faces difficulty attracting new workers, and the industry suffers from a high turnover rate because existing workers are overwhelmed with patients and aren’t getting enough support, Bufkin said.
“We are seeing enormous turnover in the state. We are seeing people not enter the field who might if wages were adequate,” Bufkin said. “We are also seeing a rotation in and out of providers because it is no longer workable for them to continue to provide services.”
Mousoom said the therapist and the psychiatrist they saw at different points both left their jobs while Mousoom was using their services. Consistent providers are important in mental health care, both they and Bufkin said.
“[Youth] are not only struggling to find care, but if they built a relationship with a provider and then suddenly that provider is no longer a part of the system, they have to rebuild that,” Bufkin said.
Role of education
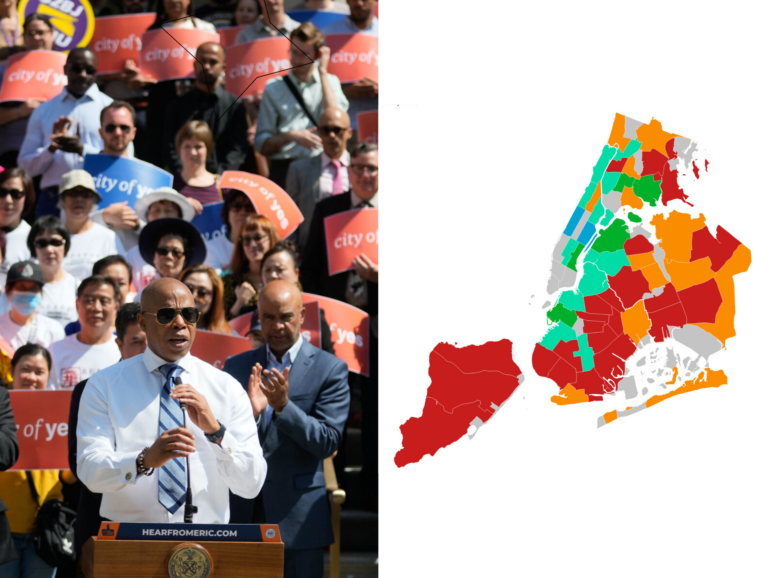
Like many of her peers, high school senior Madyson Oneiya said she has spiraled into depression recently. Oneiya–who is also a member of Students Break the Silence–said the difficulty in finding outpatient providers and encountering long waits can be discouraging for many young people, and believes more would seek help if it was more convenient to do so.
That’s why many advocates stress the importance of providing wraparound services at schools, so young people can more seamlessly access care in the same buildings where they attend classes each day. Last year, former Mayor Bill de Blasio announced that the city was hiring hundreds of additional mental health professionals to work in schools directly, pledging that every city school would have at least one full-time social worker or school-based mental health clinic.
Still, Oneiya said her school–New Explorations into Science, Technology and Math–is still prone to long lines of students seeking access to its support workers.
“We have like one counselor for each grade, or each grade group I should say, and like that really isn’t enough for everyone,” Oneiya said. “You’ll have people sitting out in the hallway waiting to see one of our counselors, forming lines, and then people will wander off because it’s not worth waiting.”
READ MORE: NYC is Expanding Resources for Students’ Mental Health. But Is It Enough?
In an emailed press release, the DOE noted that NEST+M has a 236:1 student-counselor ratio, slightly better than the 250:1 ratio recommended by the American School Counselor Association. Associate Press Secretary Suzan Sumer said all New York City public school students have access to counselors, social workers or school-based mental health clinics.
“NEST+M offers comprehensive student support through 6 guidance counselors, 1 full time social worker, and 1 part time social worker, in addition to daily and weekly social-emotional programming,” Sumer wrote in an emailed statement.
Hochul’s executive budget includes $100 million over two years for a new state matching fund to help create the Recover from COVID School Program. The program will prioritize districts with the highest needs, and allow schools to determine how funds will be spent. Ruddy said schools may use it to support mental health services, academic supports, or both.
But Oneiya also thinks adjustments need to be made to other aspects of the school environment to promote mental wellbeing. She is in a gifted and talented program, for example, so she says she has either homework or testing for just about every class, every day, and doesn’t have time to get the mental health support she needs after school.
“You don’t really have time to do anything else,” Oneiya said. “It’s a two hour commute every day. And then on top of that, two or so hours of homework or studying. You don’t really have a lot of time for anything else if you want to get sleep in.”
Martin Urbach–a teacher, dean and facilitator of the restorative justice program at Harvest Collegiate High School in Manhattan–said that addressing students’ mental health needs in schools requires a big shift in priorities.
“It will take making the curriculum be based on social emotional learning, making the curriculum be actually like, around relationship-building with students,” Urbach said. “It will definitely take a shift in what we do, how we spend time and what we prioritize what we put money to and what we put resources to.”
Tajh Sutton, the director of the youth advocacy organization Teens Take Charge, has some ideas about where money should be spent in schools. The group has been calling for resources typically spent on school policing—nearly $450 million last year—to be redirected towards school nurses and counselors, as well as arts and sports programs.
Sutton also said more money should be invested in resources to keep the school community safe during COVID.
“Some of those very basic tangible on-the-ground resources are still not meeting school communities, in the quantity and with the quality that is needed to keep people safe,” Sutton said. “I’m hearing a lot about mental health in the context of, you know, ‘kids need to be in school, they need to socialize,’ but I’m not hearing too many adults really address the valid health and safety concerns that students are bringing up.”
City Limits’ series on behavioral health and NYC’s children is supported by the Citizens’ Committee for Children of New York. City Limits is solely responsible for the content and editorial direction.








One thought on “How Will New York State’s Budget Address the Youth Mental Health Crisis?”
Yours: “Mental health always has a stigma,” Runes said. (Sandra Runes–the former director of psychological services, unit chief for the Child and Adolescent Psychiatry Service and chair of the ethics committee at Lincoln Medical Center)
The reality: We have always taught mental health has a stigma.
Harold A Maio