If and when a vaccine becomes available, legislators and health officials will have to decide how to best distribute it across the city, as well as overcome public skepticism.

Scott Housley/Centers for Disease Control and Prevention
Administering an eventual coronavirus vaccine will be a challenge, experts say, as supplies are expected to be limited at least initially.This story was produced through the City Limits Accountability Reporting Initiative For Youth (CLARIFY ), City Limits’ paid training program for aspiring public-interest journalists.
‘Legislators and health care providers will have to grapple with how to pay for it, as well as how to best widely distribute a vaccine, which will likely be scarce in its availability, at least initially.’
Ever-rising cases; state-sanctioned misinformation; stark inequities in health care. In an era where even face coverings are sources for conflict, good pandemic-related news is hard to come by. It did, however, make a rare appearance in late July when biotech company Moderna and the National Institutes of Health announced that the vaccine they’re working on entered its final phase of testing.
Much of the nation’s hopes of returning to some semblance of normal life hinge on the development of a safe and effective vaccine. But even after a COVID-19 vaccine is finalized, experts say there are a number of hurdles to successfully administering one in a city like New York.
Legislators and health care providers will have to grapple with how to pay for it, as well as how to best widely distribute a vaccine, which will likely be scarce in its availability, at least initially. The city and state will also need to overcome at least some public opposition to compulsory vaccination and skepticism of the vaccine itself, sources told City Limits.
“We’re nowhere near reaching the end of this crisis,” says Mary Beth Quaranta Morrissey, a health care attorney and researcher affiliated with Fordham University’s Global Health Care Innovation Management Center.
Logistics of distribution
The ideal vaccine, one expert says, “doesn’t need refrigeration, it is easily accessible, it is formulated well so that it can reach all areas of the country and the world.”
Though there’s no set date for when a COVID-19 vaccine is expected to become available, Raj Tiwari, professor of microbiology and immunology at New York Medical College, estimates that ideally, one could potentially be ready for distribution in a year—a timeline based on Moderna’s testing progress so far.
Even so, government officials should be preparing now for an eventual vaccine, experts say. For one, the U.S. will need to overcome its tendency to operate insularly as it attempts to develop a COVID-19 vaccine, Quaranta Morrissey says.
“Vaccine development is a collaboration among global actors––that’s the best chance of getting that vaccine developed, studied, and to market,” she says.
Tiwari believes that the State Department of Health should devote more funding towards exploring how various in-progress vaccines can actually be put into practice, focusing not just on development, but on dissemination too.
Once a vaccine is fully developed and deemed universal, there are other barriers New York will face in making it widely available to the public, including financing such a program and even the logistics of storing it.
It’s still unclear how much a COVID-19 vaccine would cost, to either individuals or governments. The Trump Administration has already spent billions on purchasing potential future vaccines from certain drug developers, and has also previously stated that it would make a vaccine free for those who can’t afford it. But a vaccine could likely be very expensive, experts say. It also needs to be physically able to withstand public distribution.
The ideal vaccine, Tiwari says, “doesn’t need refrigeration, it is easily accessible, it is formulated well so that it can reach all areas of the country and the world.”
New York has done some preparation. State Senator Brad Hoylman, who represents parts of midtown and lower Manhattan, sponsored a piece of legislation this spring that permits pharmacists and certified nurse practitioners to administer the eventual COVID-19 vaccine, aiming to speed up its delivery in response to “enormous” anticipated demand. The bill was signed into law Gov. Andrew Cuomo in June.
“As the vaccine is more widely available to the general population, that’s where I think that pharmacists can be of greater importance,” he explains.
While Hoylman is hopeful there will be a nationally-coordinated distribution effort for a vaccine, he’s concerned about logistics on a local level, including a potential lack of syringes and other medical devices needed to physically administer it to the city’s more than 8 million residents.
The ethics of scarcity
In late May, the New York State Bar Association (NYSBA)’s Health Law Section COVID-19 Task Force published a report — intended to guide policymakers and regulatory agencies as they create COVID-19-related policies — which called for the state’s Health Department to make a future coronavirus vaccine mandatory for residents (with the exception of those who receive exemptions from their doctors).
While the recommendation has already received some pushback, Quaranta Morrissey—who chaired the 13-person task force responsible for the report—believes the largest barrier to achieving widespread immunity in New York won’t be anti-vaccine sentiment, but scarcity of the vaccine itself. If there is a limited supply, lawmakers and providers must decide who gets first access to the vaccine.
“That’s where the most difficult challenges will arise,” she explains. “We are going to have to take steps to ensure that there is no discrimination in the distribution of the vaccine.”
In the event of scarcity, the report recommends prioritizing healthcare workers and other individuals who are at highest risk, both for infection and complications. It will be important for any plan to ensure equitable distribution, one that takes into account the disproportionate impact COVID-19 has had on certain groups, including Blacks.
“The inequities we’re talking about are not just disparities in healthcare, or disparities occurring now, during the pandemic,” she says. “These are inequities that are preexisting, and that the pandemic has exposed.”
The State’s Health Department says it’s currently too early to predict how a potential vaccine might be distributed across different groups, as that will depend on the specific characteristics of each approved vaccine, its availability and other factors. But scarcity is expected to be an issue.
“The New York State Department of Health continues to plan and closely monitor information from our federal partners regarding COVID-19 vaccine planning,” Department Spokeswoman Jill Montag said in a statement. “The U.S. Department of Health and Human Services has indicated that they expect that initial vaccine supplies will likely be limited.”
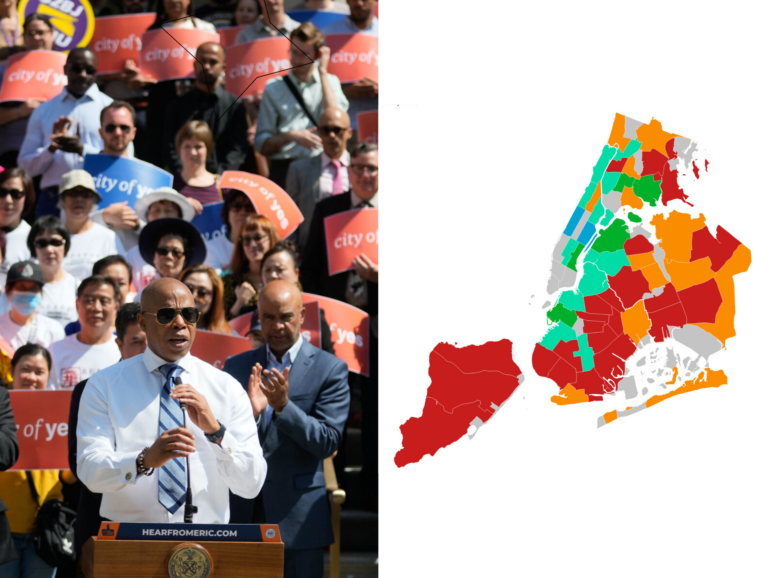
Hoylman agrees that the eventual vaccine should first be distributed to vulnerable communities — seniors, people of lower income and people of color. Targeting these communities will help eliminate the weaknesses in the healthcare system the pandemic has exacerbated, he said.
There has been a similar discussion on the national level: The Centers for Disease Control and Prevention started as early as this spring in developing a ranking system for who would get first access to a vaccine, one that would potentially prioritize essential workers and those most vulnerable, according to the New York Times.
The city’s Health Department says it will apply any future guidance the CDC provides when it comes to vaccine allocation. The city plans to distribute vaccines through its DOHMH Immunization Clinic and COVID testing sites, recruit places like urgent care centers to administer vaccines to uninsured residents and in neighborhoods with high COVID-19 rates, as well as provide extra support to health facilities in those communities.
“It’s still early but we are actively planning for an eventual vaccine and putting equity at the forefront,” City Health Commissioner Dave Chokshi said in a statement.
Public opinion and skepticism
Aside from distribution concerns, compelling all New Yorkers to receive the vaccine might also face challenges in terms of public support, as past local vaccination mandates have. Last year, driven by earlier measles outbreak, New York got rid of a prior rule that allowed families to opt out of vaccines for religious reasons, a change that angered and spurred lawsuits from those in the anti-vaccination community.
“I believe as a public official that we have to do everything in our power to make sure that we’re not allowing vaccine-preventable illnesses to take hold in our communities,” says Hoylman, who sponsored the bill to last year that repealed religious vaccine exemptions.
More than 50 state assembly members and 26 senators voted against the bill that time. They include Sen. Simcha Felder, who represents the Borough Park and Midwood neighborhoods of Brooklyn, and Sen. Brian Kavanagh, who represents parts of Brooklyn and Lower Manhattan. Felder declined a request for an interview, though said in an emailed press release that while he supports widespread vaccination, “the separation of Church and State as guaranteed by the First Amendment is a cornerstone of our Democracy.” Kavanagh also declined to comment, though a representative for his office said in an email that the senator does support vaccinations “in most instances.”
NYSBA’s report, likewise, recommends that New York offer only a medical exemption for a future COVID-19 vaccination, not religious or personal ones.
“The gravity of COVID-19,” the report argues, “presents compelling justification for State legislatures and Congress to mandate a COVID-19 vaccination.”
“We’re not dealing with normal circumstances,” Quaranta Morrisey says. “That’s called, in public health, ‘crisis conditions.’ And when you have crisis conditions, it requires a different type of approach to policy-making.”
The report cites an abundance of prior case law to support its recommendation, including 1905 United States Supreme Court case Jacobson v. Massachusetts, which held that it is within the state’s police power to mandate a vaccination. The report also notes that past, more recent legal challenges to vaccination mandates — such as healthcare workers who fought against required influenza vaccines, or parents who did not want to vaccinate their children against measles — were unsuccessful.
“All of the court decisions really take the position, if I could put it in plain language, that the right to liberty does not allow any citizen or any person to put the whole population at risk,” Quaranta Morrisey says.
But there is a vocal subset of New Yorkers opposed to the idea of a mandated vaccine: In June, some residents protested in Albany against the NYSBA report’s recommendation (NYSBA’s government body will decide whether to adopt the Task Force’s recommendations in November, a vote twice-postponed from June. But the recommendations are currently being disseminated to key policy makers.)
Among those who oppose a potential vaccine mandate is the anonymous author of the blog The Fed Up Democrat, who describes himself on the site as “a Dad from New York fighting for Freedom and Choice in New York City.” The blog’s accompanying Twitter account has more than 6,000 followers.
“It’s insanity,” the blog’s unnamed author told City Limits in an email. “There is no need to make this as-of-yet-non-existent, experimental vaccine mandatory,” he wrote. “Politicians need to stay out of my relationship with my doctor.”
New York has faced other vaccination hurdles besides skepticism: Earlier in the pandemic, public officials reported a steep drop in the number of New York City children receiving vaccines compared to last year, as many families hunkered down at home and avoided doctor’s offices.
Concerns about science
Skepticism about a COVID-19 vaccine is present nationwide: A May poll conducted by the Associated Press found that one in five Americans said they would refuse the vaccine once it was available.
A future COVID-19 vaccine has become especially contentious due to the federal government’s emphasis on rapid testing and distribution: Operation Warp Speed aims to deliver 300 million doses of a COVID-19 vaccine by January, prioritizing speed as well as newer testing methods. Some worry such measures will make a future vaccine riskier and less reliable, given that a vaccine normally takes around a decade to develop.
Tiwari believes that a public education program about vaccines should be implemented as early as high school, in order to combat misinformation about their safety and ensure that young adults understand the benefits of getting vaccinated.
Similarly, Quaranta Morrissey says that New York undertaking a linguistically and culturally-responsive educational campaign — one of the Health Law Section report’s three main recommendations — will be key to building public acceptance for a future COVID-19 vaccine. Resistance in the U.S. to vaccinations is due in part to “a lack of understanding of the science.”
“We’re seeing the marginalization of science in the response in some quarters to the pandemic,” she says.
In a statement, Health Commissioner Chokshi acknowledged these realities and says the city is prepared to work with communities to overcome potential vaccine concerns, pointing to its handling of last year’s measles outbreak in Brooklyn.
“As the Health Department prepares for an eventual COVID-19 vaccine, we know there are critical steps we need to take, including addressing vaccine hesitancy and developing distribution capacity in hard-hit neighborhoods,” he said.
“Last year, this agency faced down the worst measles outbreak in three decades and we know the importance of trusted community partners to reach New Yorkers who may be hesitant.”








One thought on “Even After a COVID-19 Vaccine is Approved, Distribution Will Be Challenging”
Our reusable gown canada remaining light and breathable, the face mask features slip-on, convenient ear loops to ensure secure closure. A full-width nose piece is also built into the mask for a more comfortable fit. The isolation mask can also be used over any other face masks and respirators for additional protection.