
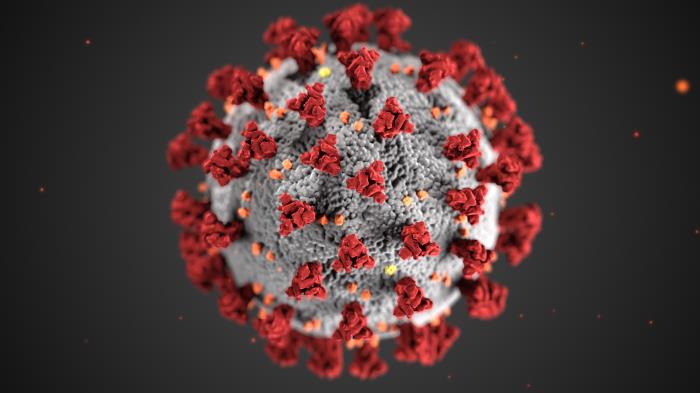
CDC
More than a month after health officials began sounding alarms about a potentially fatal illness among children who had been exposed to COVID-19, New York’s tally of known cases of the disease stands at 207, with three fatalities.
Those numbers are dwarfed by the case-count and death toll the coronavirus itself has racked up since mid-May. COVID-19 has claimed the lives of 15 people aged 19 or younger in New York State.
“Considering the number of kids who have likely been exposed, [MIS-C] is definitely not a common condition,” says Dr. Rachael Piltch-Loeb, an associate research scientist at the NYU School of Global Public Health and a preparedness fellow at the Harvard TH Chan School of Public Health.
But Multisystem Inflammatory Syndrome in Children (MIS-C), which has also been referred to as Pediatric Multisystem Inflammatory Syndrome (PIMS), remains a topic of intense discussion among health professionals. The state Department of Health on Thursday held a third webinar for providers about the syndrome. Experts say much remains unknown about the condition and the type of threat it poses.
“Since the beginning of the COVID-19 pandemic I think that one of the cautions has been that this is not only new but it’s constantly evolving,” says Dr. Danielle Laraque-Arena, the senior scholar-in-residence at the New York Academy of Medicine.
What the numbers mean
MIS-C is characterized by inflammation in the heart, kidneys, digestive tract or other organs. According to the U.S. Centers for Disease Control and Prevention, symptoms include fever, abdominal pain, vomiting, diarrhea, neck pain, rash, bloodshot eyes and intense fatigue. Clusters of cases have been reported in multiple U.S. states as well as Italy, France, Switzerland and the United Kingdom. Many of the children hospitalized for it have required intensive care.
The relatively low number of cases of MIS-C could reflect the nature of the condition as well as its novelty. While there is now an official set of criteria for diagnosing MIS-C cases and a requirement that they be reported to the state, MIS-C is not defined by one prominent symptom but by a host of possible problems, some of which are common ailments in kids. It’s possible pediatricians are missing some cases, or that the job of reporting it falls into the cracks between the multiple specialists who might treat a particular case.
What does seem clear in the cases so far is that kids with MIS-C recently had the coronavirus. In New York State, 94 percent of kids with MIS-C have tested positive as having an active COVID-19 infection or having developed antibodies to COVID-19. Whether the remainder developed the syndrome from some other cause, or whether they just received a false negative on their COVID-19 test, is unclear. “We don’t know if it’s the accuracy of the test,” or something else, says Dr. Maria Lyn Quintos-Alagheband, the chief quality officer for children’s services at NYU Winthrop Hospital and an associate professor of pediatrics at NYU Long Island School of Medicine.
Who gets it?
It appears kids who display MIS-C were either asymptomatic or mildly ill with COVID-19 before the more serious symptoms set in. Little else is known about factors—race, ethnicity, blood type, genetic predisposition—that might affect a child’s risk of getting it. It’s also unclear whether underlying conditions might play a role in how the syndrome affects a child, but so far most MIS-C patients do not exhibit any of the pre-existing conditions that made adults more vulnerable to COVID-19. “They were well—absolutely fit and well,” Laraque-Arena says.
“These are relatively healthy children. In adults [with COVID], there’s a lot of complication and co-morbid conditions,” but not in kids, says Quintos-Alagheband, although she cautions, “Until we see final data, it’s hard to say if there is an association.”
As new as it is, the fact that MIS-C seems very closely linked to COVID-19 means it is less mysterious than the disease it mimics, Kawasaki, whose cause remains unknown. The exact nature of the linkage between COVID-19 and MIS-C is uncertain, however.
“It appears to be an excessive immune response to previous virus exposure,” says Piltch-Loeb. “It’s unclear if it’s a response to the immune system creating antibodies or to the virus itself.” If MIS-C is related to the immune response to COVID-19, it would hardly be the first childhood illness with that feature: It’s an immune response that makes untreated step throat develop into rheumatic fever. “It’s not uncommon for kids to have a delayed response because their immune systems are still developing so rapidly,” Piltch-Loeb adds.
What to worry about
Children with MIS-C are not contagious. And the vast majority get better. “The prognosis is for recovery, and they recover very quickly,” Quintos-Alagheband says. “Parents should be aware of the symptoms because early diagnosis and management can lead to favorable recovery.” If symptoms appear, she recommends a visit with a pediatrician.
The more children who are seen, says Laraque-Arena, the more will be learned about the details and dangers of the illness.
MIS-C or PMIS gives parents another acronym to worry about when the 2020-2021 school year begins in September. But when it comes to the risks posed by contact with other children, it is likely that defending against the syndrome requires the same steps as protecting against the coronavirus itself.
“I’m not sure PMIS has to enter the calculus for reopening schools because we have to think about that as a COVID-19 problem,” says Piltch-Loeb. “If we reduce the chances of getting COVID-19, we reduce the risk of PMIS in the population.”









One thought on “Lots of Unknowns Remain About COVID-Related Illness that Sickens Kids”
How many children in that age group died around the same time of the year in 2019 and 2018? How many of these children had had flu vaccinations and what percentage had had all their vaccinations?