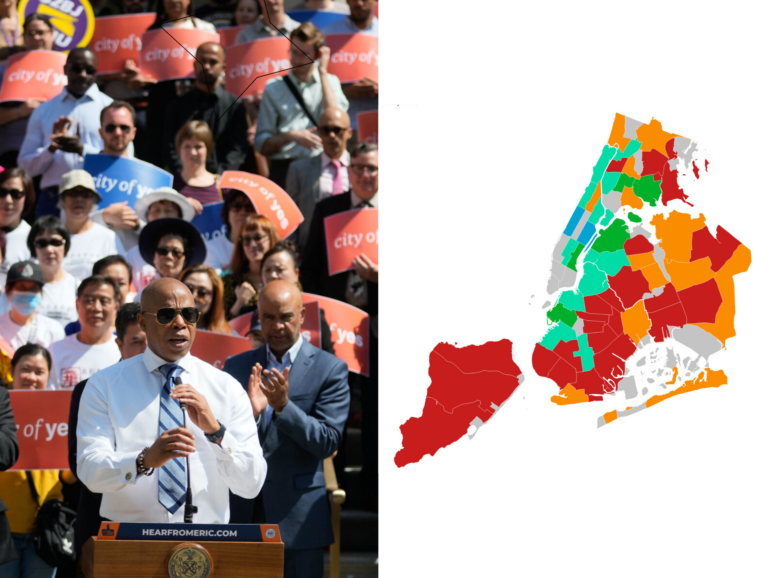
Photo by: Marc Fader
Sofia Acosta assists Madeline Hendricks, a Bronx resident with colon cancer.
Though unemployment remains north of 9 percent in the “post-recession” city economy, there are a few bright spots for New Yorkers seeking work. If you’re a computer programmer or network systems analyst, for example, the state labor department projects that businesses will still be hiring for the foreseeable future. Or you could take advantage of the number one growth industry: home health aides, which are expected to add a whopping 5,230 jobs a year statewide. By 2016, according to the state’s projections, nearly 300,000 New Yorkers will be employed as home health caregivers, either as health aides or in the related field of “personal and home care,” which includes caregivers for the elderly or infirm who don’t handle medication.
For those without advanced technical skills thinking of a career change, there’s only one problem: Though demand for home care aides—who do everything from cooking and cleaning for home-bound patients to bathing and dressing them—is soaring, wages remain dismal. The average wage for home health aides nationwide, according to a recent study by the National Employment Law Project, is only $10 an hour, less than what’s needed to clear the poverty line for a family of four with full-time work—and many home care workers are limited to part-time hours. Furthermore, according to NELP policy co-director Annette Bernhardt, that’s not counting a huge “grey market” of home aides working off the books after their state-funded hours have run out, who can earn as little as $2 an hour.
“When you look at occupations, I think home care workers and child care workers are really rock bottom,” says Bernhardt. Home care, she notes, is the only occupation that annually appears on both the lists of total jobs added and the percentage rate of increase. “This is such an incredibly critical sector—and it’s got some of the worst jobs in the economy.”
In many ways, home care aides are the poster children for New York’s new working poor. One in seven low-wage workers in New York City is currently a home care worker, according to Carol Rodat, New York policy director for the Bronx-based direct-care advocacy group PHI National. It’s also one of the most frequent referrals for welfare-to-work programs: According to the city Human Resources Administration, 12 percent of its job placements are as home health aides, narrowly trailing “sales” for the number one spot.
Yet despite the ubiquity of home care jobs in a still-weak employment market, some job developers try to avoid placing their clients there, because of the often-dismal working conditions and wages. The median wage for home health care in New York state overall is $10.66 an hour, slightly above the national average. According to Rodat, however, most workers in the city—where the living wage law enacted in 2002 applies only to personal care workers, not health aides—earn $8.50 an hour or less, and many must resort to food stamps and other benefits to make ends meet. And assigned hours may fluctuate wildly from month to month, with the result that even a living-wage job can sink to poverty level in an eyeblink.
The reasons why are buried deep in the bureaucratic tangle of Medicaid reimbursement rates and home health licensees and subcontractors that are particular to New York state. Following the nursing-home scandals of the 1980s, New York state ramped up its licensing and funding of home care agencies as an alternative way of providing care for the elderly. “For years, running a licensed agency was viewed as a small business opportunity in this state, and the Department of Health used to help people open these agencies,” says Rodat.
The result, even some home care operators say, is a mishmash of contractors and subcontractors that is weighed down with too many layers of bureaucracy and insufficient oversight of how public money is spent. Though Medicaid pays $18 an hour for a home health aide, much of that can be siphoned off by intermediate contractors and subcontractors before it ever reaches the aides themselves, says Michael Elsas, president of Cooperative Home Care Associates, a worker-owned and cooperatively run home care agency in the Bronx.
“Home care workers are sometimes referred to as ‘transient,’ which drives me nuts,” says Elsas, noting that by providing guaranteed hours and benefits, his company is able to keep its employee turnover rate below 20 percent a year. According to Rodat, turnover throughout the industry—once as high as 40 percent annually thanks to poor wages and high burnout—has fallen to less than 24 percent thanks to the lack of other job options, helping create a worker glut that has made it harder for aides to find enough hours.
Even labor organizing has had only a limited impact on home care wages: More than 70,000 home care workers in New York are members of the union 1999 SEIU, but according to Bernhardt, even a strong union is no match for the lack of Medicaid money available. “1199, that’s one of the highest density organized sectors in the country is home care workers in New York,” she says. “But their wages are still not anywhere near as high as unions can get wages when they’re in a service sector industry. It’s just because the dollars aren’t there.” (1199 officials did not respond for comment by press time.)
Rodat and Elsas call for more transparency in the state’s home care contracting, so that New Yorkers can at the very least see how their Medicaid dollars are being spent. (Currently only state payments to contractors are tracked, not subcontractors or workers themselves.) Beyond that, Rodat would like to see contracting reform to where providing a living wage for home care workers carries as much weight as keeping rates down. “The fundamental underlying motivation right now in home care is to get the cheapest that you can,” she says. “We have to change it 180 degrees and say that’s not the basis on which we want people going into someone’s home to take care of them.” Other options include consolidating contracts to cut out smaller operators with lower economies of scale, and reassigning tasks that currently require certified nurses to home care aides, potentially freeing up Medicaid money for wage increases.
Elsas, for his part, holds out hope that as more people reach the age where they’re likely to need home care, they’ll create the political pressure for reform. Or as he puts it: “Baby Boomers want what they want. And Baby Boomers don’t want to go into nursing homes.”
Randall Wilson, a home care expert at the Boston-based Jobs For the Future, agrees, but notes that fundamentally, “there’s a mismatch between the rate of government reimbursement to third-party entities and agencies, and what the actual costs are to provide the care.”
And with Medicaid cost savings already at the top of the national and state health care agendas, that could bode ill for increased funding for home care. “Because of long-term Medicaid money issues, and the demographics of an aging population, it’s going to be difficult,” admits Wilson. “And it’s very difficult to solve this problem without finding a way to improve reimbursement. That’s the conundrum.”