WhiteHouse
The Trump administration has said it’s open to states making waiver requests, but so far it seems like it only will entertain requests that fit the administration’s ideology.
A year ago, the Cuomo administration announced it would seek a waiver from the feds to provide Medicaid coverage 30 days before release to prisoners with significant mental or physical health issues.
But a day before President Donald Trump’s inauguration, the state withdrew its request. With a new administration and new leaders at the Department of Health and Human Services (HHS) and Centers for Medicare & Medicaid Services (CMS), the Cuomo administration was nervous that this request, and another request related to covering New Yorkers with AIDS, would open the door for the feds to meddle with New York’s existing Medicaid program.
Some criminal justice reformers see the waiver withdrawal as a sign that years of progress in providing better access to health services for released prisoners will come to a halt under President Trump. And with the possibility of Obamacare repeal and changes to Medicaid expansion funding, they fear hard-fought reforms to re-entry services in New York are in jeopardy.
“We were headed in a direction that for decades we’ve known precisely what needed to be done: You want it to be a seamless release,” says Ann Jacobs, director of Jon Jay College of Criminal Justice’s Prisoner Reentry Institute. “To have the work, at best on hold, and really jeopardized, is tragic in a lot of ways.”
Getting prisoners on Medicaid 30 days prior to release would have been a game changer for re-entry services with national implications. The program would have potentially saved the state millions while ensuring ex-inmates had no gap in the coverage they needed for drug abuse and mental health services —without which, officials say, some may relapse or reoffend and end up back behind bars.
But state officials were worried about the power of the feds to change its existing Medicaid program and try to leverage this request with other changes to Medicaid like drug testing recipients or work requirements, something states with Republican legislatures or governors are excited about. This new request was technically an amendment on the longstanding waiver that New York already has with the feds, so officials didn’t want to jeopardize its existing program.
“That’s what made us so nervous,” says Jeff Helgerson, the state’s Medicaid director. “There’s such wide authority for the secretary of Health and Human Services to designate that authority down to the CMS commissioner.”
The Trump administration has said it’s open to states making waiver requests, but so far it seems like it only will entertain requests that fit the administration’s ideology.
“Given some of the rhetoric coming from the new administration and their expressed interest in things like mandatory drug testing linked to Medicaid eligibility, mandatory work requirements, things we really have no interest in here in New York, we decided to pull back on those amendments,” says Helgerson. “Our concern is that they would attempt to leverage this act into a more fundamental change to the program that would affect millions.”
Though this initiative is closely related to getting drug treatment and the nation’s opioid epidemic, something Trump has said he would end, Helgerson wasn’t entirely optimistic that the Trump administration would embrace it.
“The issue is that, in essence, this could be viewed as a Medicaid expansion,” Helgerson says.
“On the one hand, they talk about better access to care for people with opioid addiction challenges,” says Helgerson. “And at the same time they seem hell-bent on trying to cut Medicaid and take away health insurance from people.”
Seamless re-entry
The goal of the waiver is to fix a longstanding problem in prisoners re-entering society with access to health services.
While behind bars, prisoners are not allowed to receive health services paid for through Medicaid. States and local municipalities are responsible for inmates’ care while they are behind bars. But when they exit prison — especially since Medicaid expansion covers an estimated 80 to 90 percent of New York’s prison population — their path to health care is usually going to the feds. This transition can leave returning citizens with a gap in coverage. And that gap can mean returning citizens cannot access medication, critical mental health services, methadone or other federally-approved substance abuse treatments, drug counseling or general health care.
“What often happens is that an individual is back in the community trying to access services and the Medicaid system erroneously thinks that this individual is still in jail,” says Tracie Gardner of Legal Action Center, which worked with the state on the waiver request and has been advocating for better access to services for released prisoners for decades.
“If you get them stabilized as they are leaving, it portends for a better outcome, and ideally, less relapse and recidivism as they continue being in the community after release,” adds Gardner.
“That transition can be a really critical time,” says Gardner. “Many people who have gone into jail or prison with opioid addiction stopped using while they were in jail or prison, but when they get out, they use again and they are overdosing.”
State officials say if they could get prisoners with significant mental or physical health issues — including drug treatment programming — on Medicaid 30 days prior to release, there would be no gap in coverage and transitioning back to society would be easier with less of a risk of relapse or reoffending.
“The program would ensure a smooth transition back into society for thousands of formerly incarcerated individuals and help reduce the rate of relapse and recidivism in communities across the state,” read Cuomo’s press release from last year.
Chipping away at ‘inmate exclusion’
This waiver is the latest in a long line of exceptions to the decades-old rule that if you are behind bars, Medicaid can’t pay for your health care, which has been around since the inception of the program.
In 1997, the feds said inmates who leave prisons or jails for at least 24 hours to receive treatment in local hospitals are eligible to get their bills paid, at least in part, by Medicaid. This saved states, including New York, millions, and even more after Medicaid expansion because more inmates are covered. This also applies to juvenile inmates who are moved from a prison to a psych facility, which New York also does. Thirty-one states and the District of Columbia also no longer terminate prisoners from Medicaid when they are behind bars, instead suspending them so when they exit prison it can be more easily turned back on.
Other states have requested waivers to get better coverage for inmates while saving money. In December, Connecticut became eligible for federal Medicaid funding for inmates that they parole to a community nursing home.
Jacobs says she’s worried about the gains that were made.
“There’s always a change when you get a new mayor, a new governor, or a new president. You know they always think that the people before them didn’t know very much, but they don’t willfully go about dissasembling things in the way that this federal administration has done,” she says.
The Cuomo administration has said they may reintroduce the waiver after they speak with federal Medicaid officials.
Gardner was optimistic that it would get enacted under Trump, “because it’s a good idea,” but says an even larger issue is if the Affordable Care Act is repealed and Medicaid expansion funding is turned into block grants.
New York’s justice-involved population has benefited greatly from Medicaid expansion. In the past five years, federal Medicaid funding to New York increased by $8.7 billion or 35 percent, in large part due to expanding Medicaid coverage to childless adults under 65 living up to 133 percent of the poverty level. That included a lot of ex-prisoners, so in 2014 New York began an initiative to get as many inmates walking out of prison on Medicaid. Last year, the state Department of Corrections and Community Supervision enrolled more than 8,000 people as part of its Medicaid enrollment program.
New York City has made a similar effort. In 2016, approximately 55 percent of those entering a New York City jail had Medicaid and the city’s Health and Hospitals Corporation submitted more than 2,600 Medicaid applications for those who didn’t.
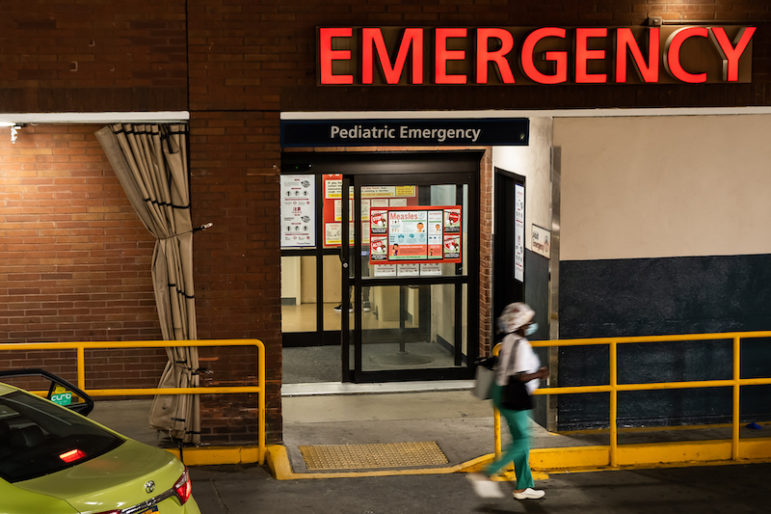
“Providing healthcare to the re-entry population reduces healthcare costs by avoiding expensive emergency room visits and helps reduce recidivism,” says DOCCS Spokesman Thomas Mailey.
If the feds were to cap Medicaid spending, as Speaker Paul Ryan has vowed to do, New York would lose billions in funding — and a lot of poor New Yorkers would no longer have access to health services when they leave prison and return to communities.
Asked what the impact on New York’s justice-involved population would be if the ACA were repealed and Medicaid were block granted, Gardner says it would be “awful.”
“Devastating,” she says. “Just devastating.”