People living in group settings, like homeless shelters, are at particular risk because of the higher likelihood for skin-to-skin contact and because the virus can spread through clothing, towels and bed sheets used by people with monkeypox, health officials say.
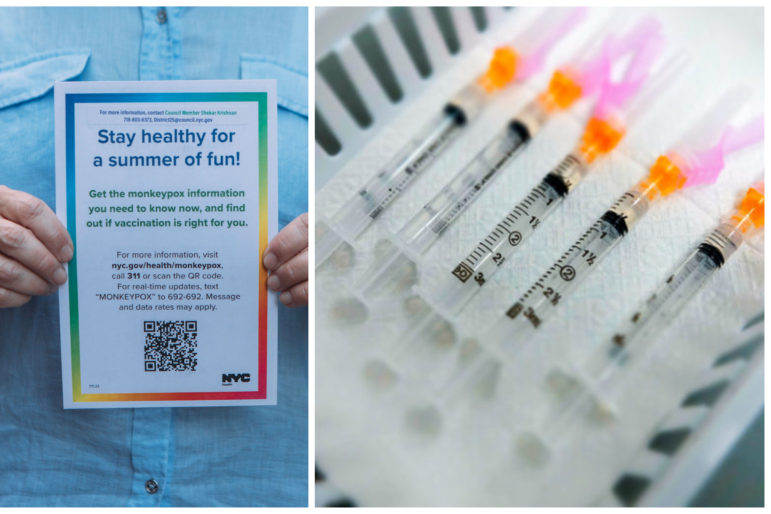
Right: Emil Cohen/NYC Council; Left: NYS Governor’s Office
Since May, at least 2,620 people statewide—2,431 of them in the five boroughs—have been diagnosed with monkeypox.As federal health officials warn of the risk of monkeypox transmission inside congregate shelters, New York City has opened a handful of nonprofit-run isolation beds for homeless residents who test positive for the highly contagious, highly painful virus.
The city’s Department of Health and Mental Hygiene (DOHMH) last month tapped the organization Comunilife to reserve six beds in its medical respite program for people with monkeypox living in homeless shelters or public spaces.
So far, 11 people have used the beds since DOHMH issued the contract in early July, said Comunilife Executive Vice President Michael O’Donnell. All 11 were men, mostly men of color, and patients stayed in the isolation beds for between seven to 20 days, O’Donnell said. None of the isolation rooms are currently in use, he added, though at one point five of the six beds were filled.
O’Donnell said it was unclear whether all 11 of the patients referred to Comunilife were homeless. But guidance shared with hospitals and viewed by City Limits specifically states that to be eligible for the isolation program, patients must have a “confirmed positive or highly suspected monkeypox case” and live in or otherwise be discharged into “a dormitory-style shelter,” another type of congregate setting with shared bedrooms, or be “street homeless or undomiciled.”
Patients must also be 21 or older, test negative for COVID-19, manage their own medication and be “psychiatrically stable enough to accept and receive care and not disturb others,” the referral form continues.
Hospital staff have to complete the form for homeless New Yorkers to get into the Comunilife isolation program, though it may take 24 hours to determine their eligibility, according to documents shared with City Limits. In the meantime, the patients may have to be admitted to a hospital to wait for placement.
“The Isolation Bed Program provides short-term self-isolation space to support rest and recovery in a safe environment,” the form states, adding that patients may have to share a double room. “Every attempt will be made to isolate patients in single rooms.”
O’Donnell said Comunilife’s six available rooms each have a single bed. The agency’s current emergency contract expires soon, but Comunilife hopes to secure another deal for four beds with the ability to open additional isolation rooms on a per diem basis if the need arises, he said.
“We don’t have the referrals flowing through yet, but the assumption is that we’ll need more [capacity],” he said. “Everybody is anticipating that.”
The Department of Homeless Services (DHS) said a handful of clients have so far tested positive for monkeypox, but did not specify how many. At a Council hearing Aug.9, Department of Social Services Commissioner Gary Jenkins, who oversees DHS, said the agency is collaborating with DOHMH and the city’s public hospital system.
“Monkeypox as you know is rising and we are working with DOHMH and [Health + Hospitals] to identify isolation for those individuals if they do indeed have monkeypox,” Jenkins told Councilmember Crystal Hudson.
A DHS spokesperson said the agency is also working with private hospitals to refer people for isolation. Clients who present with symptoms of monkeypox, such as sores in their mouth or around their genitals, are referred to a hospital or health clinic to be examined in a private setting, they added.
Since New York City recorded its first known case of monkeypox in late May, at least 2,620 people statewide—2,431 of them in the five boroughs—have been diagnosed with the illness, which causes painful lesions and is transmitted through direct contact with the sores of an infected person or with items, like clothing, that touched the sores. New York state has accounted for about 20 percent of the roughly 12,000 confirmed cases across the U.S., federal health data shows.
Monkeypox is almost always non-fatal but typically causes a painful rash, as well as fever, chills and other flu-like symptoms that can last up to four weeks. A person is still considered infectious until their rash fully heals and is replaced by a new layer of skin.
The illness has so far predominantly affected men who have sex with men, illustrating the risk of transmission through close physical contact with an infected person, but can infect anyone.
President Joe Biden declared monkeypox a public health emergency earlier this month, with vaccine rollouts hindered by crucial errors and delays at the federal level. A treatment medication known as TPOXX is available to alleviate symptoms, especially for people who are immunocompromised and more likely to become extremely ill.
People living in group settings, like homeless shelters, are at particular risk because of the higher likelihood for skin-to-skin contact and because the virus can spread through clothing, towels and bed sheets used by people with monkeypox, according to the Centers for Disease Control and Prevention (CDC). Monkeypox can also spread through respiratory particles during lengthy face-to-face contact.
The CDC and National Healthcare for the Homeless Council encourage institutions to move infected individuals off-site if they do not have access to a private room with a dedicated bathroom and a door that closes.
The CDC also urges clear communication about monkeypox transmission with staff and residents—guidance that may be going unheeded across New York City’s sprawling shelter system. Four shelter residents interviewed by City Limits Tuesday said they have not heard or seen any information about monkeypox in their facilities.
Ron Brynaert, an independent journalist who lives in a shelter in The Bronx, said everything he has learned about monkeypox has come through the media.
“There’s no signs, no warnings, no nothing in the shelter,” Brynaert said. “But if I thought I had it, I would go to my doctor and they would tell me. Then I would call the facility and see if I would lose my bed.”
Samuel Irving, a resident of another large men’s shelter in The Bronx, said staff have not circulated warnings or guidance about monkeypox either. He said he has not seen any information posted in the shelter, as was common early and throughout the COVID-19 pandemic. “There’s nothing on the walls,” he said.
DHS did, however, send directions to nonprofit shelter providers about isolating residents with probable cases of monkeypox and for referring people for medical care last month. Unlike with COVID-19, DHS will not use commercial hotels to isolate individuals with monkeypox, according to the three-page document shared with City Limits by two shelter administrators.
Instead, the guidance instructs staff to temporarily isolate clients with monkeypox and send them back to the hospital if they test positive there but attempt to reenter the shelter. The agency’s internal medical unit will contact DOHMH to seek a referral for isolation in the case of clients who return to the shelter after receiving a diagnosis at a medical clinic.
Shelter residents who share a unit with their family members and who have a private bathroom may remain in that unit, the DHS guidance continues. And two people with monkeypox can be isolated in the same room, according to the document, mirroring federal health guidance.
DOHMH and the Greater New York Hospital Association (GNYHA) hosted a webinar about the Comunilife referral process for providers on Aug. 11. A GNYHA spokesperson declined to share the webinar video, saying that doing so would violate the trade group’s internal policies.
Dr. Betty Kolod, a primary care physician and leader in New York Doctors Coalition, which advocates for better healthcare services for homeless New Yorkers, said she had not heard of the Comunilife program and doubted whether word had spread among other medical providers.
Traditionally, she said, patients are referred for the respite program only after they are admitted to a hospital.
“Many physicians are not aware of medical respite as an option and it is prohibitive to have to admit a person to the hospital in order to get a person into medical respite,” said Dr. Betty Kolod. “I’d be surprised if many people knew this was an option.”
A DOHMH spokesperson said that referrals to the Comunilife program can come directly from hospitals or from other medical providers who first contact the Health Department’s provider access lines.
Other advocates for homeless New Yorkers say the Comunilife respite beds appear to be a positive isolation strategy, but they worry what would happen if the program becomes overwhelmed.
Shelly Nortz, the deputy executive director for policy at the Coalition for the Homeless, said she was aware of four cases of confirmed or suspected monkeypox among shelter residents. At the time, she said, DHS was providing isolation rooms in their shelters.
“Comunilife is better than what we had previously,” she said, adding that limited dwindling shelter space could complicate isolation protocols. “The larger capacity crisis is cutting this one too close to the margins.”
Catherine Trapani, the head of Homeless Services United, which represents shelter providers, said the current isolation strategy has not been explained to every organization.
“They haven’t made it clear how much capacity they have,” Trapani said. “The provider is the one holding the bag while all that is worked out and they’re left to hope and pray they don’t get a suspected case in the meantime.”







