In a state accustomed to boasting about the breadth of its public health insurance system, Governor Pataki’s proposed $1.6 billion in Medicaid cuts have struck a deep nerve. It was, after all, just a couple of years ago that New York triumphantly expanded Medicaid in ways no one had seriously attempted since Lyndon Johnson inaugurated the program nearly four decades ago.
But it was only a matter of time before New York’s celebrated Medicaid system–and the national network it is part of–hit the wall. Facing rising numbers of uninsured and seeing no sign of broad national health care reform, Medicaid planners throughout the country expanded their systems in recent years by building a house of cards. The recession jump-started the collapse, and now a Bush administration plan will likely finish it.
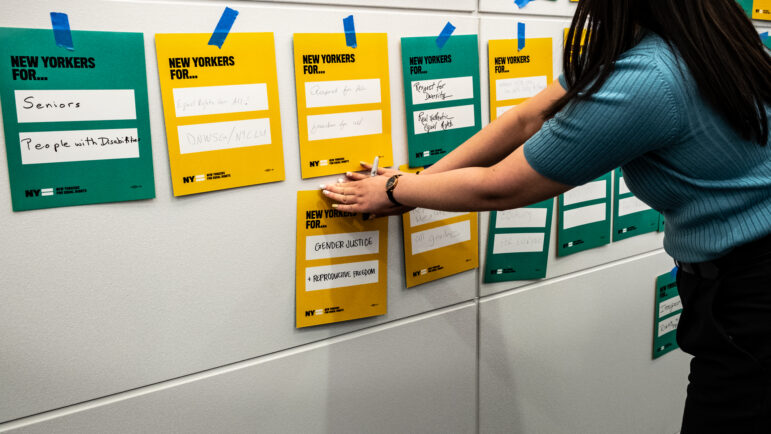
Medicaid grew out of nearly 50 years of Democratic presidential efforts to create a public health insurance system. Each failed, until the Democrats won lopsided control of Congress in 1965, allowing Johnson to usher in Medicaid and Medicare. The idea was to first offer basic health care to poor women, kids, seniors and people with disabilities, then slowly grow into a national health insurance system.
But Washington reneged on its promise of growth. Not until the 1990s, after Bill Clinton’s health care reform efforts failed, did Medicaid really expand. That growth, however, did not result from the sort of lasting policy changes that Johnson pulled off. Instead, state governors and the Clinton administration dealt with a hostile Congress by focusing on short-term growth–since 1998, enrollment has gone up by seven million people–at the expense of long-term stability.
Medicaid is an entitlement program, meaning that federal funding is determined by need. The law dictates which categories of people states must cover. It also specifies what benefits the states must offer and how to do so. In return, Washington pays a proportion of the costs, no matter how high they get. If a state wants to do anything beyond what federal law stipulates, it has to get permission. And any permanent changes to Medicaid requirements have to be legislated by Congress. This has annoyed governors for decades.
But the administration can authorize rule-bending “demonstration projects” that are supposed to be pilots for reform. In the program’s early days, rule bending was rare, but the Clinton administration changed the game by encouraging states to apply for waivers. Governors were delighted, but they were also told that waivers would be approved only if they expanded coverage. Today, more than one-fifth of Medicaid funding is spent on demonstration projects.
The catch-22 is that demonstrations must be “budget neutral”–meaning they can’t cost more than what the feds would spend without the waivers. So states submitted applications that predicted budget neutrality: they said innovations would save money, and the savings would fund expansion. Would prediction become reality? The answer was left for another day.
The Bush administration has brought us to that day. In January, Secretary of Health and Human Services Tommy Thompson proposed turning Medicaid into a block grant program, in which Congress fixes an annual payment for each state, and any further cost is the state’s problem. In return, states will get what Thompson calls “carte blanche” to design much of their Medicaid programs the way they see fit.
Thompson’s proposal lets each state switch to Bush’s block grant or stay with the traditional entitlements. But the choice is not quid pro quo. States that choose the new block grants will be eligible for some of the $13 billion funding boost the White House is proposing over the next seven years. States that stick with the old entitlements, however, will have to lobby Congress to increase the feds’ share of a program that already costs $280 billion a year.
Thompson says that when freed from the “straitjacket” of federal rules, states will come up with new ways to save money without hurting care. That’s the same idea that supported Clinton-era waiver mania. But here’s what both approaches ignore: Medicaid is not a wasteful program; it’s just expensive. The only real way to trim costs is to cut services or pay less for them–and the only sustainable way to expand the program’s reach is to support people’s right to health care, and commit financially to that right.
_______
When states started applying for waivers, their first and most popular innovation was managed care–which gives a health care provider a fixed payment for promising an enrollee treatment, regardless of how frequently or infrequently he or she actually uses the service. One of Medicaid’s biggest challenges has been reducing beneficiaries’ reliance on expensive emergency room visits for routine care, a practice that drives up costs and makes preventive health care more difficult. In a 1997 Urban Institute study, 44 percent of adults had been to the ER in the previous year. Managed care promises stability. By assigning patients to a primary care provider, it promotes a long-term doctor-patient relationship and controls costs.
Today, 49 states have varied Medicaid managed care plans. New York’s is among the most far reaching. It was Governor Pataki’s central health care reform, and it has been slowly expanding each year since Washington approved the idea in 1997. In 2001, New York also established Family Health Plus, extending insurance to families making up to one and a half times the poverty level and even to childless adults living at the poverty level.
This expansion, however, has little to do with any savings that might have stemmed from managed care. The United Hospital Fund is completing a five-year study evaluating costs and quality of treatment after New York’s managed care conversion. So far there’s little hard data, so researchers have turned to piecemeal surveys of providers. “What came out of that,” says Katherine Haslanger, who is leading the study, “is a sense that not much has changed” in terms of monetary savings or better-quality care.
What Haslanger calls the “eligibility noise” of Medicaid–the constant monitoring of whether beneficiaries in fact qualify–cancels out the stability of managed care. Every six months, Medicaid applicants have to verify over 20 factors about their lives, ranging from income to family size. These details often change, leading to disqualification. So enrollees cycle in and out of the system, undermining the long-term doctor-patient relationship the health plans are supposed to promote. According to one United Hospital Fund study, only 42 percent of people who enrolled in 1998 kept 12 months of uninterrupted coverage.
New York’s system suffers from yet another profound flaw: providers also cycle through quickly. So most health plans are sponsored by hospitals. But hospitals’ primary care providers are their outpatient clinics, where residents–doctors in training–comprise nearly half the staff, according to the United Hospital Fund survey. Residents finish their training and leave.
The first states to embrace managed care, in the early 1990s, soon discovered how expensive it really was. Even in the best of circumstances, an effective enrollment process requires sustained outreach and case management early in the program. Getting private health plans to participate means paying rates that are high enough to attract and retain them. Haslanger’s review of other states’ experience found that none reaped the fanciful 5 to 10 percent savings first predicted for managed care. Indeed, few states still bother to promote their managed care systems as cost cutters. “New York is much more the exception,” says Stephen Zuckerman of the Urban Institute. And as Pataki’s proposed budget cuts make clear, New York is one more state that can no longer cling to the “cost-cutter” notion.
_______
Managed care’s economic failures weren’t important during the economic boom years when states expanded their systems. Governors felt flush with money from soaring tax revenues and from public assistance loads trimmed by welfare reform. Encouraged by Washington, states felt safe to open their Medicaid systems the way Pataki did in New York, even when savings from managed care never materialized. But with the recession lingering now, the Bush plan gives states creative ways to shrink rather than expand their systems. For example, a state could offer prescription drugs only to patients with certain illnesses, or deny enrollment to people with health problems that cost a lot to treat. Granted, federal law would still make all states do some things, but these fixed policies would account for only 35 percent of all Medicaid spending. Under the Bush plan, one-third of current Medicaid enrollees would get no protection from federal rules.
Moreover, Medicaid’s big growth area, cost-wise, comes from providing long-term care for elderly and disabled folks, and prescription drugs for everyone. Spending on elderly and disabled enrollees accounts for three-quarters of costs nationally. Prescription drugs comprised nearly one-fifth of all Medicaid costs between 1998 and 2000, according to the Kaiser Family Foundation. Under the Bush plan, states that can’t economize with innovations like managed care will have to either cut drug coverage or stop paying for long-term care.
Neither option is palatable. That’s likely why governors are in a wait-and-see mode. Congress must approve Bush’s plan, but it is also considering a handful of bills that would simply expand the federal share of Medicaid costs next year, easing some immediate budgetary pressures.
If the Bush plan wins out, states will likely claim the $13 billion additional funding over the next seven years. But there’s a catch. In keeping with Medicaid’s reform habit, the Bush plan is budget neutral over 10 years. As a result, states that opt for quick relief will have to pay it back in a decade–via reduced funding. Is anyone thinking about this, or are the governors of one mind with Thompson? When a reporter asked him about the 10-year payback, he answered mirthfully: “I’m not going to be here to solve that problem.”